Deep in the central part of the skull is one of the most anatomically complex bones of the skeleton - the sphenoid (main) bone, in the body of which is the sphenoid sinus (also called the main or sphenoidal). Unlike the other three air sinuses (maxillary, frontal and ethmoid), the sphenoid sinus is not paired, although it is divided by a septum into two asymmetrical parts. Located above the nasopharynx, the sphenoidal sinus belongs to the posterior paranasal tract. Thanks to small holes (fistulas), it communicates with the so-called sphenoidal pocket, and then with the upper nasal passage.
Causes of sphenoiditis
Sphenoiditis or sphenoidal sinusitis is an acute or chronic inflammation of the mucous membrane of the main cavity.

The causative agents of the disease are infections: viruses, fungi, bacteria (mainly staphylococcal and streptococcal).
That is, sphenoiditis can be the result of influenza, tonsillitis, or even simple, untreated rhinitis. However, in comparison with other paranasal sinuses, in acute respiratory diseases, the area of the main cavity is least susceptible to inflammatory processes and, in case of damage, quickly returns to normal. In order for disease-causing organisms to begin to exert a destructive effect in this department, certain conducive conditions are necessary:
- anatomical narrowness or small size of the anastomosis;
- abnormal development during the formation or changes due to trauma (absence or overgrowth of ducts, curvatures, additional septa);
- the emergence of all sorts of formations (polyps, cysts, tumors);
- ingress of foreign bodies with a sharp breath (due to too wide anastomosis).
Features of the course of sphenoiditis
 In most cases, an infection that provokes inflammation of the mucous membrane in the sphenoid sinus gets there from other paranasal sinuses or nasal and pharyngeal cavities (often from the nasopharyngeal tonsils). In the presence of the above conditions, which lead to a narrowing of the communicating outlet, air movement is impeded and the infection is in a favorable environment for progression.
In most cases, an infection that provokes inflammation of the mucous membrane in the sphenoid sinus gets there from other paranasal sinuses or nasal and pharyngeal cavities (often from the nasopharyngeal tonsils). In the presence of the above conditions, which lead to a narrowing of the communicating outlet, air movement is impeded and the infection is in a favorable environment for progression.
The consequence of prolonged inflammation is infiltration and edema of the mucous membrane, followed by blockage of the excretory duct.
In addition, anaerobic infection can develop due to oxygen deprivation, which contributes to the appearance of pus.
As a result, with complete blockage of the duct, purulent discharge can completely fill the sphenoid sinus.
Much less often, the infection penetrates into the main cavity due to damage to the sphenoid bone. This happens with the bony form of syphilis, tuberculosis or osteomyelitis.
Destroying the main bone, the infection gradually penetrates into the thickness of the mucous membrane, causing inflammation and edema.
In addition, sphenoiditis can also occur without direct contact of pathogenic organisms with the mucous membrane. With prolonged inflammation of the nasopharynx against a background of reduced immunity and without proper drug treatment, there is a risk of severe swelling of the nasopharyngeal mucosa. This edema, in turn, clogs the anastomosis of the sphenoid sinus from the outside, preventing normal air exchange. Carbon dioxide accumulating in the cavity begins to have a destructive effect on the mucous membrane, as a result of which the inflammatory process begins.
Symptoms of sphenoiditis
It is not easy to diagnose sphenoiditis, since the disease often proceeds without pronounced specific symptoms. However, the lack of treatment can have serious consequences. The fact is that the wedge-shaped sinus is located in dangerous proximity to such anatomical structures as the pituitary gland, hypothalamus, optic nerves and carotid arteries. Through the upper and lateral walls of the sinus, pathogenic organisms can penetrate into the cranial cavity and cause serious disorders, including optic neuritis, meningitis or brain abscess.
Among the main symptoms of sphenoiditis are:
- headache;
- neurological (asthenovegetative) manifestations;
- mucopurulent discharge from the nose or along the back of the throat;
- impairment of smell and vision.
Headache often becomes the first clinical manifestation of sphenoiditis. The accumulation of fluid and air in the main sinus, as well as toxin infiltration due to prolonged inflammation, contribute to an increase in pressure on bone structures and tissues.
 Depending on the degree of blockage of the sinus outlet duct, the patient may be disturbed by moderate to high intensity pain. As a rule, at first, patients complain of constant aching pain in the center of the head, but over time it is localized in the occiput. Unpleasant sensations may increase in conditions of higher ambient temperatures and dry air. If the headache is a symptom of sphenoiditis, it cannot be relieved with pain relievers.
Depending on the degree of blockage of the sinus outlet duct, the patient may be disturbed by moderate to high intensity pain. As a rule, at first, patients complain of constant aching pain in the center of the head, but over time it is localized in the occiput. Unpleasant sensations may increase in conditions of higher ambient temperatures and dry air. If the headache is a symptom of sphenoiditis, it cannot be relieved with pain relievers.
In addition, sphenoiditis can manifest itself through asthenovegetative symptoms such as:
- decreased appetite;
- dizziness;
- memory impairment;
- sleep disturbance;
- slightly elevated temperature (37.1 - 37.9 degrees);
- weakness and malaise.
Such manifestations of the disease are due to the fact that the sphenoidal cavity is in close proximity to the structures of the central nervous system. Due to prolonged inflammation and destruction of mucosal cells, numerous toxins enter the nerve tissue of the base of the brain and thereby cause the above symptoms.
As for the pathological discharge, they appear in the patient due to the accumulation of infected fluid in the main sinus. As a rule, mucous masses are first secreted, and then, with the development of infection, purulent discharge appears, which, seeping through the outlet, drain along the back of the pharynx. Drying, purulent discharge turns into crusts, so patients often complain of discomfort in the depths of the nasopharynx and try to clear their throat. In addition to unpleasant sensations, a person may smell or taste in the mouth.
Finally, patients often complain of impaired sense of smell and vision. When the inflammatory process goes beyond the sphenoid sinus, it is able to affect the olfactory receptors in the nose and fibers of the optic nerves.
As a result, a person may stop correctly perceiving smells and lose visual acuity or feel double vision.
Diagnostics of the sphenoiditis
With persistent headaches and mucopurulent discharge from the nose or along the wall of the pharynx, the patient should consult an otolaryngologist. The doctor should examine and interview the patient to identify additional symptoms of sphenoiditis. An effective method for diagnosing the disease is rhinoscopy, which allows you to examine the nasal passages, the mucous membrane of the nasal cavity, the vault of the pharynx and the surface of the soft palate. For the diagnosis, computed tomography is also done, which with high accuracy displays the state of all paranasal sinuses.
Treatment and surgery for sphenoiditis
The next steps of an otolaryngologist after diagnosing sphenoiditis are: elimination of the causative agent of the disease, removal of edema of the mucous membrane and anastomosis, and improvement of the outflow of the main sinus.As a rule, the doctor prescribes to the patient both systemic (in the form of injections or tablets) and local (in the form of drops) antibiotic therapy. To relieve swelling, vasoconstrictor drops are often taken.
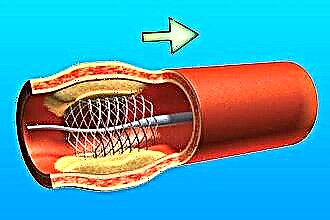
If conservative methods of treatment do not bring the desired result, then the treatment is accompanied by surgery.
 Endoscopic surgery allows the specialist to freely approach the sinus anastomosis, expand it and sanitize the cavity. However, since the infection itself does not play a decisive role in the development of sphenoidal sinusitis, an operation to restore the deviated septum of the main sinus may be required.
Endoscopic surgery allows the specialist to freely approach the sinus anastomosis, expand it and sanitize the cavity. However, since the infection itself does not play a decisive role in the development of sphenoidal sinusitis, an operation to restore the deviated septum of the main sinus may be required.
Based on the fact that any sinusitis, including sphenoidal sinusitis, mostly occurs against the background of a weakened immune system, doctors usually recommend also paying attention to strengthening the body's immune system.
Cystic lesions in the wedge-shaped sinus
In addition to sphenoidal sinusitis, the appearance of cystic formations in it has a negative effect on the main cavity. And although most often cysts form in the frontal (80%) and ethmoid (15%) sinuses, in 5% of cases they still affect the maxillary and sphenoid sinuses.
This happens when the ducts of the glands of the mucous membrane are clogged and the secret they produce accumulates in the gland, expanding its walls.
Over time, this clot turns into a cyst. Its contents can be: mucous (in most cases), purulent, serous and airy.
Diagnosis and symptoms of wedge-shaped sinus cyst
A sphenoid sinus cyst is rarely detected immediately after its appearance, since it can only be detected by computed tomography of the paranasal sinuses or brain structures. In this case, even regular examinations by an otolaryngologist will not help to make a diagnosis. The situation is also complicated by the fact that often the disease (especially at first - for several years) is almost asymptomatic.
 The main clinical manifestations of cystic pathology of the sphenoidal sinus include:
The main clinical manifestations of cystic pathology of the sphenoidal sinus include:
- headaches in the occipital region;
- dizziness and nausea;
- sinus pressure;
- visual impairment.
Since over time the cyst grows and begins to press on the mucous membrane and walls, the sinus gradually stretches, and pathological changes occur, which can affect and have a negative effect on adjacent anatomical structures.
Treatment of cystic pathologies in the sphenoid sinus
Nowadays, in addition to surgical removal, drug treatment of cystic pathologies is also used. However, effective therapy is possible only in the early stages of the disease. Due to the absence of symptoms, patients, as a rule, do not immediately learn about the existence of a cyst and seek medical help when the neoplasm reaches an impressive size. In addition, drugs only help slow down the growth of the cyst, but they do not completely cure the pathology and do not prevent the risks of relapse. Thus, the most effective method of treatment is surgical removal using endoscopic equipment.
Surgical intervention occurs only if the patient has pronounced symptoms or there is a threat of complications. Provided that, in the opinion of an otolaryngologist, the cyst does not interfere with the normal functioning of the sphenoidal sinus and the disease proceeds without symptoms, it is not necessary to remove the neoplasm. In this case, the patient needs to be regularly monitored by an ENT doctor.