Febrile fever, chest pain and excruciating cough are the main symptoms of tracheitis. In adults, tracheitis quite often joins the inflammation of the bronchi, pharynx and nasal cavity, as a result of which patients are diagnosed with combined diseases - laryngotracheitis, rhinopharyngotracheitis, etc. Allergic forms of pathology in 97% of cases develop against the background of an allergic rhinitis or conjunctivitis.
Febrile fever, chest pain and excruciating cough are the main symptoms of tracheitis. In adults, tracheitis quite often joins the inflammation of the bronchi, pharynx and nasal cavity, as a result of which patients are diagnosed with combined diseases - laryngotracheitis, rhinopharyngotracheitis, etc. Allergic forms of pathology in 97% of cases develop against the background of an allergic rhinitis or conjunctivitis.
Tracheitis is not a dangerous disease, but if not treated promptly, it can cause laryngeal stenosis or bronchial obstruction.
Etiopathogenesis
The provocateurs of inflammatory reactions in the tracheal mucosa are often staphylococci, pneumococci, Pfeifer's bacillus and influenza virus. The overwhelming majority of infectious agents are unstable in the environment, therefore, infection occurs mainly through contact with a carrier of pathogenic flora.
According to observations, tracheitis very rarely develops as an independent disease. The mucous membranes of the lower airways are often affected against the background of acute bacterial and viral infections - tonsillitis, flu, scarlet fever, pharyngitis, sinusitis or frontal sinusitis. Inflammation of the trachea can be caused by:
- hypothermia;
- dysbiosis;
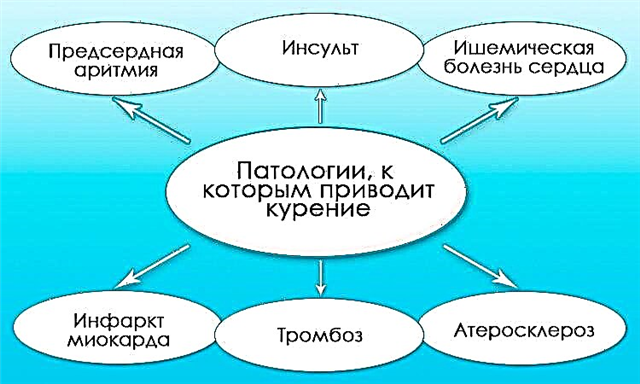
- tobacco smoking;
- contact allergens;
- inhalation of dry air;
- burns of mucous membranes;
- dustiness of the air.
Tracheitis is more susceptible to people suffering from somatic pathologies - rheumatism, cirrhosis of the liver and diabetes mellitus.
It is worth noting that the allergic form of the disease often develops against the background of septic, especially bacterial, inflammation of the respiratory tract. Some types of gram-positive microbes (streptococci, pneumococci) can cause allergies and, as a result, severe edema of the ciliated epithelium in the trachea. In such cases, patients are diagnosed with infectious-allergic tracheitis, which most often becomes the cause of life-threatening complications.
Types of tracheitis
How does tracheitis manifest in adults? The clinical manifestations of the disease depend on the rate of spread of the infection. With a sluggish course of septic inflammation, the symptomatic picture is weak. In this regard, there are two types of tracheitis:
- acute - the symptoms of the disease are pronounced and appear within a few hours after infection of the trachea; with adequate and timely therapy, inflammation can be completely eliminated within 10-14 days;
- chronic - a sluggish, and often lifelong, inflammation of the mucous membranes of the upper respiratory tract, characterized by periods of relapse and remission.
With a sluggish inflammation, morphological changes occur in the structure of the ciliated epithelium, which covers the inner surface of the trachea. Depending on the characteristics of the course of pathological processes, two forms of chronic disease are distinguished:
- hypertrophic - characterized by thickening of the walls of the tracheal mucosa and an increase in the amount of mucus produced, as a result of which patients develop a spastic wet cough;
- atrophic - thinning of the walls of the ciliated epithelium, which leads to the formation of dry crusts on the surface of the trachea and, as a result, a painful dry cough.
In the stage of remission, chronic tracheitis practically does not manifest itself in any way. However, with a decrease in immune defense, inflammation exacerbates, which causes a spastic cough.
Signs of tracheitis
What are the first signs of tracheitis? Dry spastic cough and low temperature are characteristic symptoms of the development of ENT disease. The attacks are most often exacerbated at night and immediately after waking up. A suffocating cough can be provoked by deep breaths, frosty air, laughing or screaming.
With a favorable course of the disease, after 2-3 days in the bronchi and trachea, mucus liquefies and begins to evacuate from the respiratory tract during coughing. If the causative agents of infection are pyogenic bacteria, impurities of pus may be found in the sputum. After seizures, patients complain of a burning sensation in the chest and a sore throat.
 As the infection progresses, symptoms of intoxication appear - muscle pain, nausea, lack of appetite, weakness, apathy. In patients prone to allergies, inflammation of the trachea leads to severe swelling of the mucous membrane. In this regard, signs of respiratory failure may appear - inspiratory shortness of breath, heart palpitations, wheezing during breathing, etc.
As the infection progresses, symptoms of intoxication appear - muscle pain, nausea, lack of appetite, weakness, apathy. In patients prone to allergies, inflammation of the trachea leads to severe swelling of the mucous membrane. In this regard, signs of respiratory failure may appear - inspiratory shortness of breath, heart palpitations, wheezing during breathing, etc.
If the inflammation is left untreated, the infection will descend into the tracheobronchial tree and cause complications. Especially often with severe pathology, patients develop pneumonia and bronchiolitis.
Symptoms of acute tracheitis
Signs of acute inflammation of the trachea occur following an infectious lesion of the overlying parts of the respiratory tract. Symptoms of tracheitis are nonspecific and are very similar to those of laryngitis. At first, an unproductive cough appears, which intensifies with talking and taking a deep breath. In this regard, patients try to breathe shallowly so as not to provoke irritation of the mucous membranes.
Other manifestations of the acute form of ENT pathology include:
- elevated temperature;
- noisy breathing (stridor);
- burning sensation in the chest;
- sore throat;
- malaise;
- hoarseness of voice;
- cardiopalmus;
- intercostal retractions;
- difficulty swallowing;
- lack of appetite;
- dry, spastic cough.
Initially, coughing can occur exclusively at night, but if untreated, attacks periodically occur during the day. As a rule, the general condition of the patient suffers slightly. Mucus during seizures practically does not separate, but 4-5 days after infection of the trachea, the cough becomes wet. Purulent and sometimes bloody impurities are found in the sputum. Most often, this indicates ulceration of the ciliated epithelium and rupture of small blood capillaries in the throat.
In some cases, the bronchi are affected simultaneously with the trachea, as a result of which the clinical picture changes slightly.
Cough attacks become more frequent and longer. Patients begin to complain of a lack of oxygen and tachycardia. All this signals the development of tracheobronchitis, which can provoke airway obstruction and bronchopneumonia.
Bronchopneumonia that develops in old age can be fatal.
Symptoms of fungal tracheitis
Fungal forms of ENT disease develop mainly against the background of pharyngomycosis or tonsillomycosis. The causative agents of infection are opportunistic fungi, which begin to multiply actively only if local immunity is reduced. Symptoms of tracheal inflammation depend on which fungus caused the pathological reactions in the respiratory tract:
| Type of fungal infection | Infection routes | Clinical manifestations |
|---|---|---|
| actinomycosis | a fungal infection enters the mucous membranes of the ENT organs from the esophagus | fungi provoke the formation of tumors in the respiratory tract, resulting in symptoms of respiratory failure - shortness of breath, heart palpitations, stridor; in the places of localization of pathogens, scar tissue can form, therefore, with actinomycosis, complications often arise in the form of stenosis of the larynx |
| candidiasis | yeast-like fungi penetrate into the trachea from the oral cavity, larynx, gastrointestinal tract | in addition to spastic cough and shortness of breath, patients complain of itching in the pharynx, an allergic rash on the skin and mucous membranes, burning in the chest and between the shoulder blades, low-grade fever |
| aspergillosis | the infection enters the upper respiratory tract from the bronchi | due to an allergic reaction to fungal metabolites, a runny nose, cough and fever occur; when coughing up in sputum, yellow accumulations are observed, which signals the presence of pus in the mucus; in rare cases, bronchial spasm occurs during attacks, as in bronchial asthma |
In case of mycotic (fungal) damage to the trachea, antifungal drugs of systemic action are used. They inhibit the reproductive function of fungi, thereby reducing the severity of inflammation and symptoms of the disease.
Chronic tracheitis symptoms
Chronic tracheitis most often manifests itself with inadequate treatment of the acute form of the disease. The provocateurs of sluggish inflammation of the respiratory tract are bacteria, more often streptococci. Spastic hacking cough and subfebrile fever are the main manifestations of sluggish tracheitis in adults.
Attacks occur mainly at night with abundant secretion of mucopurulent sputum. As already mentioned, in chronic inflammation, either hypertrophy or thinning of the ciliated epithelium is observed. Both forms of the disease pose a health hazard and can provoke complications.
 Symptoms of chronic tracheitis can be exacerbated against the background of such provoking factors:
Symptoms of chronic tracheitis can be exacerbated against the background of such provoking factors:
- tobacco smoking;
- inhalation of dust;
- allergy;
- hypothermia;
- toxic poisoning.
During periods of exacerbation, the clinical manifestations of the disease do not differ from the symptoms of acute tracheitis. Sluggish inflammation of the respiratory tract leads to severe intoxication of the body.
Due to the accumulation of toxic substances in the tissues, the patient's condition worsens over time, nausea, headaches, myalgia (muscle pain), etc. intensify. It is possible to completely eliminate the manifestations of the disease when taking antimicrobial drugs, in particular sulfa drugs. On average, the entire course of treatment takes 10-14 days, subject to all the recommendations of the ENT doctor.
Local manifestations of tracheitis
In the acute course of the disease, edema, infiltration and hyperemia (redness) of the ciliated epithelium are observed. Viscous mucus forms on the surface of the trachea, which liquefies over time and is evacuated from the respiratory tract during forced exhalation, i.e. coughing. In the case of a viral infection of the respiratory tract, traces of blood may be found in the sputum, which indicates a hemorrhagic rash on the walls of the respiratory system.
As a rule, with atrophic tracheitis, the inner surface of the throat becomes grayish.
The mucous membranes become crusted, which irritate the throat and provoke a spasmodic dry cough. In the hypertrophic form of the disease, a strong expansion of the blood vessels is observed, as a result of which the ciliated epithelium acquires a bright red color.
If we take into account the fact that tracheitis most often develops against the background of other respiratory diseases, concomitant local manifestations include:
- swelling of the palatine arches;
- redness of the larynx;
- soreness of the lymph nodes;
- slight hypertrophy of the glands.
The rapid spread of bacterial and fungal infections can lead to the development of lymphadenitis. With a fungal infection of the respiratory tract, the formation of a white curdled plaque on the walls of the pharynx is not excluded. In connection with allergic reactions on the skin, pinpoint rashes may appear, provoking itching or burning.
Subglottic tracheitis
If inflammation is observed only in the upper part of the trachea, i.e. directly on the border with the larynx, patients are diagnosed with subglottic tracheitis. The symptoms of the disease are identical to those of acute laryngitis. Inflammation of the mucous membranes is most often indicated by:
- hoarseness of the voice;
- labored breathing;
- burning sensation in the throat;
- Barking cough;
- aphonia.
The vocal cords are often involved in the infectious process, as a result of which voice disorders occur. In the absence of therapy, the voice may disappear altogether or drop by several tones. Intense voice loads during an exacerbation of the disease can cause irreversible processes leading to aphonia. To prevent complications, the patient must strictly observe vocal rest.
Inflammation of the vocal cords and larynx increases the risk of stenosing. Swelling of the glottis leads to respiratory failure and the development of a false croup. Attacks of a suffocating cough, accompanied by hypoventilation of the lungs, can provoke fainting and acute asphyxia, i.e. suffocation.
Even when undergoing examination by an ENT doctor, it is not always possible to distinguish subglottic tracheitis from laryngitis. However, pathologies are treated according to the same principle, therefore, with the timely administration of drugs, the inflammation quickly regresses and the patient is recovering.
Symptoms in pregnant women
Tracheitis in pregnant women in most cases develops against the background of acute respiratory viral infections and hypovitaminosis. A decrease in the body's immune defense entails the multiplication of pathogenic agents and, as a result, inflammation of the upper or lower parts of the respiratory tract. The main symptoms of the development of ENT pathology in expectant mothers include:
- malaise;
- nausea;
- subfebrile condition;
- lack of appetite;
- sore throat;
- spastic cough;
- stomach ache;
- nasal congestion.
Coughing fits lead to high blood pressure and uterine tone, which can lead to miscarriage in early pregnancy.
If the inflammation is not controlled, it can lead to abnormal development of the fetus. The fact is that bacterial and viral infections are able to overcome the placental barrier and infect the child's body. A neglected respiratory disease can undermine the health of not only the expectant mother, but also her child.
The difficulty lies in the fact that the infection quickly descends into the lower respiratory tract, provoking the development of pneumonia and bronchitis. To prevent serious consequences, you need to seek help from specialists when the first signs of inflammation of the ENT organs appear.