In most cases, pathology occurs in children under 5 years of age, since it is at this age that the tissue of the pharyngeal space undergoes involutive modifications.
In most cases, pathology occurs in children under 5 years of age, since it is at this age that the tissue of the pharyngeal space undergoes involutive modifications.
ENT disease in adults is predominantly secondary in nature and develops against the background of chronic inflammation of the tissues of the oropharynx, tuberculosis, sluggish tonsillitis, neck injury, etc.
Abscess therapy involves the prompt opening of abscesses, followed by the use of medication and physiotherapy.
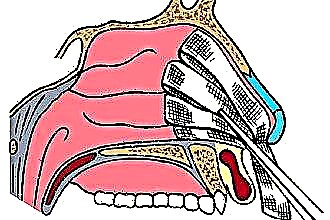
A little about anatomy
What is an abscess and why is it most often diagnosed in children? The retropharyngeal space is a gap filled with connective tissue, which is located between the prevertebral and muscular fascia. The fiber is crossed by a connective tissue septum that begins in the prevertebral fascia and ends in the pharynx. The septum divides the pharyngeal region into two parts, which prevents the penetration of pus from one part of the space to another.
In children under 5 years of age, lymph nodes are located near the connective tissue septum, which “collect” lymphatic fluid from the middle ear and nasopharynx cavity. With the penetration of the pathogenic flora into the lymph nodes, the infection with the blood stream spreads throughout the pharyngeal region, which entails the formation of a purulent abscess. In adults, these anatomical structures are absent, therefore, they are much less often diagnosed with the so-called. "Retropharyngeal abscess".
Pathogenesis
The reason for the development of ENT pathology is the reproduction of pyogenic microbes (hemophilic bacillus, meningococci, streptococci). With the defeat of the pathogenic flora of the mucous epithelium of the nasopharynx, an infectious-allergic reaction develops. Over time, neutrophils, leukocytes, granulocytes and other immunocompetent cells penetrate into the foci of inflammation. They secrete special biologically active enzymes into the fiber, which stimulate the expansion of small and large capillaries.
When introduced into inflamed tissues, neutrophils absorb pyogenic microorganisms, after which they die. It is they, with elements of neutralized microbes, that form a purulent exudate in the tissues affected by inflammation. To limit the spread of pus, leukocytes accumulate near the foci of inflammation, as a result of which granulation tissue forms around the affected area. Thus, the purulent contents are contained in the connective membrane, as a result of which a large abscess is formed.
Over time, the microorganisms in the purulent exudate die, and the purulent area is opened, and the pathological secret is evacuated outside. Premature opening of the connective membrane entails the penetration of still living pathogens into the surrounding tissues, which is fraught with subsequent tissue intoxication and the spread of lesions.
Important! Untimely elimination of purulent exudate from tissues entails poisoning of the body, which is fraught with reflex cardiac arrest.
Abscess in adults
Why does a pharyngeal abscess develop in adults? Often, ENT disease in adults occurs against the background of septic inflammation of the tissues of the hearing organ and nasopharynx. Mechanical injuries leading to the destruction of the walls of the pharyngeal region can provoke purulent-inflammatory reactions and the development of pathology. In most cases, adults are diagnosed with a secondary retropharyngeal abscess, which occurs against the background of the development of the following pathologies:
- purulent rhinitis - inflammation of the ciliated epithelium in the nasopharyngeal cavity, followed by the release of purulent masses from the nasal canals; delayed relief of inflammatory reactions leads to damage to regional nodes and inflammation of the lymphoid tissues of the throat;
- sinusitis - purulent inflammation of the cavities that are located on both sides of the nose; the paranasal sinuses communicate with the pharyngeal space, therefore, with untimely destruction of pyogenic bacteria, the development of inflammation in the mucous tissues of the pharynx is not excluded;
- purulent otitis media - an infectious pathology characterized by damage to the soft tissues of the tympanic cavity; through the Eustachian tube, the pathogenic flora can penetrate into the nasal cavity and throat and provoke the development of an abscess;
- purulent pharyngitis - an infectious lesion of lymphadenoid tissues and ciliated epithelium of the oropharynx; with the progression of the disease, the epithelial tissues of the throat become covered with a white coating,
 which contains pathogenic microbes; their introduction into lymphoid tissues entails the formation of a purulent exudate and, as a result, an abscess;
which contains pathogenic microbes; their introduction into lymphoid tissues entails the formation of a purulent exudate and, as a result, an abscess; - spinal tuberculosis - destruction of intervertebral discs and bone tissue of the spine by mycobacterium tuberculosis; the subsequent accumulation of pus in the neck leads to soft tissue damage, which is fraught with the formation of abscesses in the pharyngeal region.
An injury to the neck, accompanied by damage to the tissue in the pharyngeal region, increases the risk of developing an abscess by 4 times.
Abscess in children
There are a number of infectious pathologies that are diagnosed to a greater extent in preschool children. Untimely treatment of viral and bacterial ENT diseases often leads to suppuration of the pharyngeal tissues and the formation of abscesses. Retropharyngeal abscess in children can provoke diseases such as:
- adenoiditis - bacterial or viral inflammation of the hypertrophied pharyngeal tonsil, which can lead to the spread of infection and the formation of abscesses in the pharyngeal region;
- diphtheria - a severe infectious pathology, accompanied by damage to the upper respiratory tract; toxins secreted by a diphtheria bacillus can provoke inflammation of the cervical lymph nodes, which is fraught with the development of a retropharyngeal abscess;
- sore throat - damage to the palatine tonsils by pathogenic agents, which entails inflammation of the tissues around the tonsils and, accordingly, the formation of an abscess in the pharyngeal region;
- scarlet fever - damage to the ENT organs by hemolytic streptococcus, which with blood flow can be localized in the pharyngeal tonsil and cause bacterial inflammation of the tissues;
- throat injuries - injury to the tissues of the pharynx with sharp objects (toys, solid food), which often leads to septic inflammation of the pharyngeal space.
Due to the insufficient development of adaptive (acquired) immunity, children are much more likely to be exposed to infectious lesions of the ENT organs.
In preschool children, the pathology progresses very quickly and can lead to swelling of the mucous membranes. Untimely intake of antibiotics and anti-edema drugs can lead to hypoxia and even suffocation.
Clinical manifestations
Symptoms of the pharyngeal abscess are pronounced, so it is almost impossible not to notice the development of pathology. Immediately after infection of the tissues of the pharynx, there is a sharp increase in temperature to febrile levels. Patients complain of cutting pain in the throat and painful swallowing of saliva.Against the background of general tissue intoxication, there is an increase in regional lymph nodes, a deterioration in well-being and a lack of appetite.
The classic manifestations of ENT pathology include:
- hyperthermia;
- fever;
- throat pain;
- hoarseness of voice;
- lymph node hypertrophy;
- difficulty swallowing;
- muscle pain;
- rapid breathing.
Infants become whiny and refuse to eat. The development of the disease is indicated by sleep disturbance, hyperemia of the mucous membrane of the oropharynx, swelling of the neck and profuse salivation.
Possible complications
Late treatment of a retropharyngeal abscess entails a deterioration in the patient's well-being and the development of severe local and systemic complications. Purulent tissue damage is always accompanied by severe intoxication of the body and, accordingly, an increase in the load on the detoxification organs and the cardiovascular system. Common complications after an abscess are:
 mediastinitis - an infectious lesion of the mediastinum, which entails inflammation of the lungs, large arteries and veins, heart and nerves;
mediastinitis - an infectious lesion of the mediastinum, which entails inflammation of the lungs, large arteries and veins, heart and nerves;- jugular vein thrombosis - inflammation of the walls of a large vein through which blood circulates from the tissues of the neck and cranial cavity; the formation of blood clots in the vessel leads to disruption of the trophism of regional tissues, which causes severe pain;
- asphyxia - an acute respiratory disorder, accompanied by hypoventilation of the lungs, which occurs as a result of the overlap of the airways by an abscess;
- sepsis - the penetration of pathogenic microbes into the bloodstream, which entails the development of systemic inflammation, characterized by dysfunction of vital organs;
- purulent meningitis is an infectious inflammation of the membranes of the brain, which is accompanied by severe headaches, impaired coordination of movements, seizures, impaired consciousness and stiff neck muscles.
Delayed opening of abscesses and stopping infectious processes leads to disability or death.
Lancing an abscess
What to do if the doctor diagnosed a retropharyngeal abscess? Treatment of ENT pathology is carried out exclusively in stationary conditions under the supervision of a specialist. Due to the risk of spontaneous opening of abscesses, immediately after the diagnosis is made, the patient is prescribed surgical removal of purulent exudate from the affected area.
The autopsy of abscesses in children is performed under general anesthesia, and in adults under local anesthesia. The day before the procedure, the patient should rinse the oropharynx with saline solutions to reduce the concentration of pathogens in the operated area. About 3 hours before the operation, it is undesirable to eat food, as it can enter the airways and provoke complications.
Operation progress:
- the patient is seated in a chair and covered with a sterile sheet;
- the walls of the throat are infiltrated with an anesthetic (solution of Novocaine or Lidocaine);
- after numbness of the operated area, the doctor wraps the scalpel with sterile gauze so that the length of the working part of the instrument is no more than 1 cm;
- using a medical spatula, the root of the tongue is pressed against the lower jaw;
- with a scalpel in the area of the abscess, an incision is made 1.5-2 cm long;
- after opening the abscess, the patient is tilted forward so that purulent exudate does not penetrate the airways; the wound is expanded, after which the remnants of pus and necrotic tissue are removed from the focus of inflammation;
- at the final stage, the oropharynx is disinfected with antiseptic solutions.
 On the first day after surgery, the patient should not eat food, as this creates a risk of re-development of the abscess.
On the first day after surgery, the patient should not eat food, as this creates a risk of re-development of the abscess.
After removal of the abscess, the patient is discharged from the hospital for 2-3 days, but within 20-25 days he must visit an otolaryngologist who will monitor the dynamics of wound healing.
For 5-6 days after the operation, it is recommended to gargle with a soda solution to prevent the reproduction of pyogenic microbes.
Antibiotic treatment
Antibiotic therapy is an integral part of the complex treatment of purulent inflammations in the ENT organs. After diagnosis and determination of the type of pathogen, children and adults are prescribed antimicrobial drugs. However, it should be borne in mind that exclusively drug treatment without opening the abscess will be ineffective.
For the treatment of retropharyngeal abscess, the following groups of antibiotics are usually used:
- cephalosporins ("Sulbactam", "Ceftazidim", "Cefotaxime") - inhibit the biosynthesis of cellular structures of pathogens, which leads to their death;
- lincosamines ("Dalatsin", "Klindovit", "Zerkalin") - inhibit the biosynthesis of bacterial proteins, which prevents the reproduction of pathogens;
- macrolides ("Baktikap", "Azitral", "Lekoklar") - inhibit the reproductive activity of microbes by destroying their cellular components.
Antihistamine drugs can prevent the formation of extensive edema in the pharynx. They interfere with the synthesis of cyclooxygenase, as a result of which the concentration of inflammatory mediators in the affected tissues decreases. The best anti-allergic and anti-edema drugs include Suprastin, Tsetrin, Zirtek, Egis, etc.

 which contains pathogenic microbes; their introduction into lymphoid tissues entails the formation of a purulent exudate and, as a result, an abscess;
which contains pathogenic microbes; their introduction into lymphoid tissues entails the formation of a purulent exudate and, as a result, an abscess; mediastinitis - an infectious lesion of the mediastinum, which entails inflammation of the lungs, large arteries and veins, heart and nerves;
mediastinitis - an infectious lesion of the mediastinum, which entails inflammation of the lungs, large arteries and veins, heart and nerves;