Treatment of a fungus in a child's throat should be accompanied by the intake of antimycotic (antifungal), antipyretic and anti-inflammatory drugs. The development of a fungal infection is often preceded by stomatitis, gingivitis and other inflammatory diseases of the oropharynx. In comparison with pathogenic bacteria, fungi emit significantly less toxic substances, therefore, it is not always possible to diagnose a child's disease in a timely manner. Due to the lack of specific immunity in children, the infection spreads quickly enough, affecting not only the throat, but also the palatine tonsils.
Treatment of a fungus in a child's throat should be accompanied by the intake of antimycotic (antifungal), antipyretic and anti-inflammatory drugs. The development of a fungal infection is often preceded by stomatitis, gingivitis and other inflammatory diseases of the oropharynx. In comparison with pathogenic bacteria, fungi emit significantly less toxic substances, therefore, it is not always possible to diagnose a child's disease in a timely manner. Due to the lack of specific immunity in children, the infection spreads quickly enough, affecting not only the throat, but also the palatine tonsils.
The causative agents of pharyngomycosis
How to treat a fungus in the laryngopharyngeal mucosa? The choice of the appropriate medication depends on which microorganism is responsible for the inflammation in the airways. In 76% of cases, candidal pharyngitis occurs due to the uncontrolled multiplication of yeast-like fungi of the genus Candida. They are the typical causative agents of not only fungal sore throat, but also thrush.
Much less often, a fungal disease is caused by saccharomycetes and molds, which are most often found in patients with diabetes mellitus. It should be noted that the above microorganisms are present in the microflora of the ENT organs of most healthy people. The development of pathological reactions in the mucous membranes is facilitated by a decrease in the body's resistance, which appears against the background of local hypothermia, vitamin deficiency, antibiotic abuse, exacerbation of chronic diseases, etc.
Candidal pharyngitis is not transmitted by airborne droplets or by household means, therefore sick children are most often treated on an outpatient basis.
Development features
As already mentioned, fungi that contribute to the development of fungal pharyngitis inhabit the mucous membrane of healthy people without causing them any harm. But against the background of a decrease in general or local immunity, opportunistic microorganisms are activated and begin to multiply rapidly. In the process of development, pathogens release toxic substances and waste products that provoke inflammation of the soft tissues.
Pathological reactions in the throat cause loosening of the mucous membrane and damage to small blood vessels. Over time, pathogenic fungi enter the bloodstream, as a result of which the child experiences the first symptoms of intoxication:
- lack of appetite;
- drowsiness;
- headache;
- subfebrile condition;
- nausea.
If treatment is not prescribed to the patient in time, the infection will spread throughout the body and provoke complications. Toxic substances secreted by fungi can settle in the kidneys and liver, causing inflammation and, as a result, serious diseases. Therefore, when the first signs of the disease appear, it is advisable to take the child to the pediatrician for pharyngoscopy and cultural examination of a smear from the throat, according to the results of which it will be possible to accurately determine the causative agent of the infection.
Specificity of the course of pharyngomycosis
Why are young children more likely to get sick with fungal pharyngitis than adults? The child's body is more susceptible to allergies, which negatively affects the immune defense. That is why a child is more likely to suffer from respiratory diseases than an adult. In addition, acquired immunity is practically absent in infants, so pathogens develop in the respiratory tract almost unhindered.
Pharyngomycosis can occur in two main forms:
- acute - characterized by a vivid manifestation of pathological symptoms and lasts from 7 to 20 days;
- chronic - proceeds without pronounced clinical manifestations and lasts more than 3-4 months with periodic exacerbations of inflammatory processes.
Young children are much more likely to be diagnosed with an acute form of candidal pharyngitis. But in the absence of adequate treatment, pathology can turn into a chronic form.
Pharyngomycosis classification
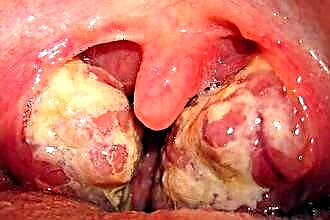
What are the symptoms of fungal pharyngitis in a child? Depending on the nature of the manifestation of local symptoms, there are several types of fungal sore throat. Some forms of ENT disease in their clinical manifestations are similar to viral pharyngitis or sore throat, however, the treatment of bacterial and fungal inflammation has fundamental differences.
In otolaryngology, it is customary to distinguish the following forms of pharyngomycosis:
- pseudomembranous - white flakes with a yellowish-gray tint are formed on the mucous membrane of the throat, which are easily removed with a spatula; sometimes under a curdled bloom, bleeding areas of the mucous membrane of a pale pink color are found;
- erythematous (catarrhal) - small spots of bright red color with a "varnished" shiny surface are formed on the walls of the throat;
- erosive-ulcerative - ulceration occurs in the places of localization of fungal pathogens and
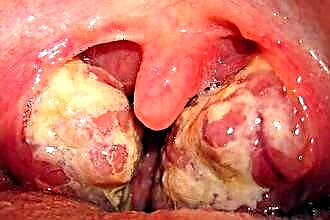 bleeding wounds;
bleeding wounds; - hyperplastic - white spots form on the surface of the mucous membrane of the laryngopharynx and the root of the tongue, which are almost impossible to separate with a spatula.
Treatment of erosive-ulcerative and hyperplastic forms of fungal disease should be accompanied by the intake of not only systemic antifungal agents, but also rinsing solutions. Throat sanitation can reduce the severity of local symptoms, eliminate inflammation and eliminate hard-to-separate curdled plaque on the walls of the laryngopharynx.
Symptomatic picture
How to recognize pharyngomycosis in a child? The acute form of the disease is characterized by a rather vivid clinical picture, while the chronic one proceeds more smoothly, but exacerbations of inflammatory processes are observed approximately 7-10 times a year. Typical manifestations of fungal pharyngitis include:
- dry and raw throat;
- discomfort when swallowing saliva;
- feeling of a lump in the Adam's apple;
- enlargement of the cervical lymph nodes;
- decreased appetite;
- chronic fatigue;
- slight increase in temperature.
Unfortunately, young children often do not pay attention to discomfort until the tickling and soreness is replaced by pain. If the child presents complaints about the state of health, it is advisable to examine the throat for inflammation and the formation of white plaque on the walls of the pharynx. Swelling of the mucous membrane, white flakes on the back of the throat, tongue and inner surface of the cheeks are clear manifestations of fungal inflammation of the respiratory tract.
During the diagnosis, the doctor must exclude the likelihood of developing diphtheria, since its symptoms are similar to the manifestations of candidal pharyngitis.
Treatment methods
What should be the treatment for fungal sore throat? The acute form of ENT disease is often treated on an outpatient basis. But in case of complications of pharyngomycosis with fungal tonsillitis or otitis media, the little patient must be hospitalized.
Therapy for candidiasis is accompanied by the administration of local and systemic antifungal agents.In order to increase the resistance of the child's body to pathogens, at the stage of resolving inflammatory processes, the child is prescribed the intake of multivitamins and immunostimulating agents of plant origin. The dosage of pharmaceutical agents largely depends on the age of the patient and the severity of the course of the infectious disease.
On average, the course of antimycotic therapy is 7-14 days in the absence of serious complications.
Therapy for fungal pharyngitis should be accompanied by the administration of medications aimed at eliminating the cause of the development of the disease, which most often include hypovitaminosis, secondary immunodeficiency and allergies.
Antimycotics
Treatment of fungal inflammation in the ENT organs in children can be accompanied by taking only safe drugs. Most antimycotics negatively affect the condition of the kidneys and liver, therefore they are not used in pediatric practice. Depending on the composition, antifungal agents are divided into several groups:
- polyenes ("Amphotericin", "Nystatin") - drugs of natural origin that damage the cytoplasmic membranes of fungi, which leads to their death;
- azoles ("Mikospor", "Intraconazole") - synthetic antimycotic drugs that destroy most strains of yeast-like and mold fungi;
- allylamines (Terbinafin, Exifin) are synthetic antimycotics, the components of which are active against not only yeast-like fungi, but also dermatophytes.
It should be understood that the treatment of candidal pharyngitis should be started even before the results of a culture study of a pharyngeal smear are obtained. For these purposes, azoles or allylamines are most often used. After determining the type of causative agent of the disease, the therapy regimen can be adjusted and supplemented with other drugs.
Local preparations
 To treat a fungus in the throat of a young child, you can use local drugs. Antifungal solutions and aerosols must be applied directly to the mucous membranes of the respiratory tract in order to accelerate the penetration of active components into the foci of inflammation. It is worth considering that topical drugs are used as an adjunct to the intake of systemic antimycotics. They only speed up the process of resolving inflammatory processes in the throat, but they do not contribute to 100% elimination of pathogenic agents.
To treat a fungus in the throat of a young child, you can use local drugs. Antifungal solutions and aerosols must be applied directly to the mucous membranes of the respiratory tract in order to accelerate the penetration of active components into the foci of inflammation. It is worth considering that topical drugs are used as an adjunct to the intake of systemic antimycotics. They only speed up the process of resolving inflammatory processes in the throat, but they do not contribute to 100% elimination of pathogenic agents.
The treatment regimen, as a rule, includes such antifungal and antiseptic agents as:
- "Natamycin" - tablets of fungistatic and fungicidal action, helping to eliminate foci of inflammation not only in the mucous membranes, but also on the skin;
- Miramistin is an antiseptic solution for rinsing the oropharynx, which inhibits the activity of yeast-like and mold fungi in the throat, palatine tonsils, gums, etc .;
- Oxyquinoline is a preparation for washing mucous membranes and treating ulcerations caused by the development of fungal flora.
The last drug must be diluted with water in a ratio of 1: 2000, since its active components can cause soft tissue burns and allergic reactions. The duration and frequency of sanitizing procedures can only be established by the attending physician after examining the child and accurately identifying the causative agent of pharyngomycosis.
Contraindications
Many antimicrobial agents can provoke an allergic reaction in a young child. For example, drugs such as "Amphotericin" and "Ketoconazole" negatively affect the functioning of the detoxification organs, i.e. kidneys and liver. Therefore, the treatment of pharyngomycosis in young children should be under the constant supervision of a specialist.
It is undesirable to give systemic antimycotics to patients suffering from renal or hepatic insufficiency. Some groups of antifungal drugs have age restrictions. In particular, allylamine medicines should not be given to children under 12-13 years old, as they cause indigestion, dysbiosis and allergic edema of the mucous membranes of the gastrointestinal tract and respiratory tract. For this reason, "Terbizin" is used in pediatric practice to treat patients aged 2-3 years.
Thus, only a specialist should deal with the selection of suitable funds and determining the dosage of drugs, since self-medication can cause the development of toxic shock syndrome.

 bleeding wounds;
bleeding wounds;