It is normal for babies to cough. It often has physiological causes and goes away on its own. A child's immunity is weaker than that of an adult, therefore, children sometimes get sick with respiratory diseases several times a year, and after them the so-called "residual cough" can last up to 2-3 weeks. Expectorant syrup for children can help the baby to cope with this problem faster. But it is necessary to give it to the child correctly, taking into account all the features of this drug.
Causes of a wet cough
A wet cough in medicine is called a productive cough. This is a protective reflex of the body, with the help of which it reacts to stimuli. A wet cough produces a large amount of mucus - and it creates the characteristic gurgling sounds. Mucus does not always come off well, and this is especially dangerous - it can accumulate in the bronchi and lungs, increasing inflammatory processes.
A moist cough rarely comes on suddenly. It usually develops into a dry, barking cough, characteristic of the early stages of respiratory illness.
However, it can be provoked by a number of other reasons:
 Allergic reaction. It is accompanied by profuse sputum production, swelling of the mucous membranes, and sometimes bronchial spasm. The child begins to cough violently, literally choking on liquid.
Allergic reaction. It is accompanied by profuse sputum production, swelling of the mucous membranes, and sometimes bronchial spasm. The child begins to cough violently, literally choking on liquid.- Chronic respiratory diseases. Most often these are sinusitis and rhinitis. In the cavity and sinuses of the nose, mucus is constantly formed, which flows down the back wall of the larynx and provokes a cough.
- Bronchial asthma. Attacks of wet cough with this disease occur mainly in the morning. During the night, the secreted secretion accumulates in the bronchi, and in the morning, with the help of a cough, the body tries to bring it out.
- Lung diseases: pneumonia, pleurisy, cystic fibrosis, tuberculosis. In most cases, they are accompanied by bouts of wet cough, often with streaks (clots) of blood or purulent discharge.
- Bronchitis. A moist cough is more characteristic of purulent bronchitis. The disease is easy to recognize by severe shortness of breath and pieces of pus, which literally fly out of the bronchi when coughing.
- Teething. The most harmless cause of wet cough in babies. The cough occurs due to the abundant secretion of saliva, which the baby simply does not have time to swallow.
The causes of a wet cough in a baby are so diverse that only an experienced pediatrician can understand them. Therefore, making independent decisions about the use of cough suppressants is at least risky.
Improper use of funds can seriously harm your baby.... Cough is not a disease, but a symptom. First of all, it is necessary to treat the underlying disease.
Dangerous symptoms
It is best to see a doctor immediately if a child's wet cough is accompanied by two or more of the following symptoms:
 a sudden, prolonged attack of a wet cough;
a sudden, prolonged attack of a wet cough;- traces, streaks, blood clots were found in the sputum;
- sputum thick, yellow or green;
- a sharp increase in body temperature up to 39-40OWITH;
- body temperature above 38OC lasts more than 3 days;
- shortness of breath, shortness of breath;
- chest pain when coughing or taking a deep breath;
- complete loss of appetite, pain when swallowing;
- wheezing in the chest, which increases with breathing;
- a wet cough does not go away for more than 3 weeks.
For a baby, 1-2 symptoms are enough to call a specialist who will examine the baby and tell you what to do next. It is likely that the child develops a dangerous disease: pneumonia, tuberculosis, purulent bronchitis, etc., which can lead to serious complications and even death.
Cough diagnostics
During the initial examination, in most cases, it is not possible to detect the true cause of a wet cough. Therefore, the doctor usually asks for a diagnostic examination, which, depending on the symptoms and severity of the condition, may include:
 general blood test - shows the presence and severity of active inflammatory processes;
general blood test - shows the presence and severity of active inflammatory processes;- analysis of mucus from the throat and / or nose - allows you to determine which type of pathogenic microorganisms triggered the disease;
- x-ray of the lungs - lesions will be visible on it in pneumonia, pleurisy, tuberculosis, bronchial dilatation with bronchitis;
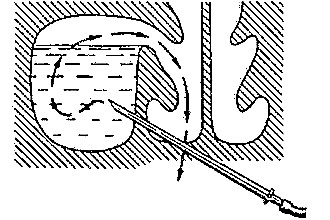
- bronchoscopy - performed in severe forms of bronchitis, allows you to examine the mucous membranes of the bronchi from the inside and take mucus for tests.
These are only the simplest standard survey methods. If the obtained data are not enough for the diagnosis, then the child may be assigned a computed or magnetic resonance imaging, a biopsy of the lungs or bronchi and other types of hardware examination.
Usually, if the doctor suspects a serious illness, then until the results of all types of examinations are received, no antitussive or expectorant drugs are prescribed to the child. Some of these can intensify coughing fits or cause bleeding from the lungs.
Types of expectorant drugs
Expectorant syrups are always only part of a comprehensive treatment. Their action is aimed at eliminating symptoms, while other drugs are prescribed to combat the underlying disease. But also coughs work in different ways. They can be divided into three large groups:
 Mucolytic. Their primary task is to change the consistency and viscosity of sputum, and to liquefy it. They are prescribed for a deep wet cough, when thick phlegm accumulates in the bronchi or lungs, and the child cannot get rid of it on his own.
Mucolytic. Their primary task is to change the consistency and viscosity of sputum, and to liquefy it. They are prescribed for a deep wet cough, when thick phlegm accumulates in the bronchi or lungs, and the child cannot get rid of it on his own.- Expectorants. Promote the rapid elimination of a large amount of liquid mucus by increasing the amount of secretion and increasing the activity of bronchial smooth muscles. It is often used after mucolytic drugs when the mucus has lost its viscosity.
- Combined drugs. They are used for severe attacks of painful cough. They combine antitussive and mucolytic properties, thus relieving the condition of the child until the mucus becomes thin enough to be easily coughed up.
In no case should expectorants be used simultaneously with antitussive drugs. This can lead to large fluid accumulation and bronchostasis.
In general, with a wet cough, antitussives are prohibited. They suppress the cough reflex, and it is needed in order to quickly remove mucus outside. Therefore, the correct choice of the drug depends not only on its effectiveness, but also on the further development of the disease.
Baby syrups
When the doctor has already decided on the diagnosis, he can prescribe a syrup to the baby to help him cough up mucus. Although most of these medicines are natural and contain extracts of useful plants, the recommended dosage must be strictly observed.
Abuse of syrup will not bring benefits to the baby, but it can provoke allergies or unwanted side reactions.
Here are some of the most effective drugs often prescribed for children:
- Mukaltin. Plant-based tablets with the strongest mucolytic effect (they gave the name to a whole group of drugs). There is syrup for the little ones.
- "Doctor IOM". A very popular remedy that at the same time looses phlegm and makes it easier to cough up. The composition includes 11 extracts of medicinal plants.
 "Alteika". An effective cough medicine based on marshmallow root. It has anti-inflammatory, mucolytic and expectorant effects, but it often provokes allergies.Give it to the child with care.
"Alteika". An effective cough medicine based on marshmallow root. It has anti-inflammatory, mucolytic and expectorant effects, but it often provokes allergies.Give it to the child with care.- "Gedelix". Another herbal preparation that uses the healing properties of ivy. It dilutes phlegm, makes it easier to cough up, promotes the transition of dry cough to wet.
- Bromhexine. A potent complex drug that effectively helps to fight cough by expanding the bronchi and stimulating their motor activity. Only a doctor can prescribe it to a baby.
- Ambroxol. Facilitates breathing, liquefies phlegm, stimulates expectoration. It has a good effect on all types of respiratory diseases. It has many analogues.
- "Licorice syrup". The drug is alcohol-based, when taken, be sure to dilute with water. Has a complex effect: anti-inflammatory, mucolytic, antiviral. In case of overdose, it causes severe side effects.
- "Fluimucil". A mucolytic drug with an expectorant effect, used for bronchopulmonary diseases as prescribed by a doctor.
- "Sinekod". Combined drug with expectorant and antitussive effect. It is prescribed for painful attacks of dry cough in order to stimulate the formation and excretion of phlegm.
- "Tussin" and its analogues. Also, a complex preparation with a pronounced mucolytic effect, softens cough, facilitates coughing.
It is good to combine the use of expectorant drugs with steam inhalation. They moisturize irritated mucous membranes, additionally provoke sputum discharge and relieve inflammation from the larynx. But for infants up to 6 months, steam inhalations cannot be done - this can cause severe swelling of the mucous membranes and an attack of suffocation.
Homemade recipes
 You can also make an effective cough syrup at home. Over the hundreds of years of its existence, traditional medicine has accumulated dozens of effective antitussive formulations. Their plus is in absolute naturalness and the ability to select components, taking into account the taste preferences and individual characteristics of the child. But in terms of their effectiveness, they are, of course, inferior to modern pharmaceuticals. Therefore, in case of serious illnesses, it is better to rely on official medicine.
You can also make an effective cough syrup at home. Over the hundreds of years of its existence, traditional medicine has accumulated dozens of effective antitussive formulations. Their plus is in absolute naturalness and the ability to select components, taking into account the taste preferences and individual characteristics of the child. But in terms of their effectiveness, they are, of course, inferior to modern pharmaceuticals. Therefore, in case of serious illnesses, it is better to rely on official medicine.
Among the simplest and most affordable homemade cough syrups are:
- Burnt sugar. It perfectly relieves sore throat and promotes good coughing up of phlegm. Simply holding a metal spoon of granulated sugar over the fire until the sugar caramelises and then pouring the contents onto the parchment will create a lollipop. And if you pour onion or lemon juice, a decoction of thyme or sage into the melted sugar in a thin stream and stir constantly, you get a semi-liquid syrup with excellent medicinal properties.
- Pine buds. They contain a high concentration of vitamins and valuable essential oils with a strong anti-inflammatory effect. Pour a tablespoon of kidneys with a glass of boiling water and simmer for 15 minutes over low heat. When the broth has cooled, strain and mix with an equal amount of honey. Take 1 tsp. 4-5 times a day.
- Propolis tincture. Helps to cope with a wet cough, even with purulent bronchitis and tracheitis, as it has antiseptic and antibacterial properties. It is divorced with water, dosage according to age is from 2-3 to 7-10 drops per half glass of warm water. Take 3-4 times a day.
- Fig milk. Boil four fresh or dried figs in milk for 15 minutes. Then beat the mixture well with a blender. Give a teaspoon 4-5 times a day. If your child is allergic to milk, you can simply boil the figs in water, but the effectiveness of the remedy will be lower.
- Black radish. A true natural healer. It has mucolytic, anti-inflammatory, antiseptic properties, increases
 immunity. The syrup is formed inside the root crop if the middle is cut out and the groove is filled with honey. Enough 1 teaspoon 3 times a day to soften the most severe cough.
immunity. The syrup is formed inside the root crop if the middle is cut out and the groove is filled with honey. Enough 1 teaspoon 3 times a day to soften the most severe cough. - Badger fat. It is difficult to call a syrup, and because of the specific taste, not every child can be persuaded to take such a medicine. It perfectly softens cough, relieves sore throat. Creates a protective film and has strong antibacterial properties.
It is desirable to supplement home treatment with natural preparations with decoctions of medicinal herbs: chamomile, sage, thyme, wild rose, linden, currant leaves. A warm drink flushes mucus from the throat, moisturizes the mucous membranes, dilutes phlegm and dilates the bronchi.
The toxins and decay products of drugs formed during illness are also excreted in a dissolved state, so the amount of water drunk by a child per day should be at least a liter.
When treating a wet cough, it is necessary to constantly monitor the condition of the baby. If the course of therapy is selected correctly, then the cough usually goes away in a week, maximum - in 10-14 days. The residual cough can last as long. But he is no longer accompanied by profuse sputum and seizures should not be. If the cough continues for a month or more, it is likely that the disease has become chronic and a second visit to the doctor is imperative. Otherwise, the development of complications cannot be avoided.

 Allergic reaction. It is accompanied by profuse sputum production, swelling of the mucous membranes, and sometimes bronchial spasm. The child begins to cough violently, literally choking on liquid.
Allergic reaction. It is accompanied by profuse sputum production, swelling of the mucous membranes, and sometimes bronchial spasm. The child begins to cough violently, literally choking on liquid. a sudden, prolonged attack of a wet cough;
a sudden, prolonged attack of a wet cough; general blood test - shows the presence and severity of active inflammatory processes;
general blood test - shows the presence and severity of active inflammatory processes; Mucolytic. Their primary task is to change the consistency and viscosity of sputum, and to liquefy it. They are prescribed for a deep wet cough, when thick phlegm accumulates in the bronchi or lungs, and the child cannot get rid of it on his own.
Mucolytic. Their primary task is to change the consistency and viscosity of sputum, and to liquefy it. They are prescribed for a deep wet cough, when thick phlegm accumulates in the bronchi or lungs, and the child cannot get rid of it on his own. "Alteika". An effective cough medicine based on marshmallow root. It has anti-inflammatory, mucolytic and expectorant effects, but it often provokes allergies.Give it to the child with care.
"Alteika". An effective cough medicine based on marshmallow root. It has anti-inflammatory, mucolytic and expectorant effects, but it often provokes allergies.Give it to the child with care. immunity. The syrup is formed inside the root crop if the middle is cut out and the groove is filled with honey. Enough 1 teaspoon 3 times a day to soften the most severe cough.
immunity. The syrup is formed inside the root crop if the middle is cut out and the groove is filled with honey. Enough 1 teaspoon 3 times a day to soften the most severe cough.