A nebulizer is a device that sprays a drug into an air suspension. The use of nebulizers can significantly increase the bioavailability of the drug, since when inhaled, 98% of the aerosol gets directly to the site of the lesion.
 At the same time, this provides economic feasibility - to obtain the necessary therapeutic effect, much less drug should be spent, since it does not dissipate.
At the same time, this provides economic feasibility - to obtain the necessary therapeutic effect, much less drug should be spent, since it does not dissipate.
In addition, the creation of suspension in the nebulizer occurs without the use of additional propellant gases.
That is why nebulizer inhalation with a wet cough, as well as with a dry cough, is considered the best method of delivering medicine to the respiratory system.
Which nebulizer should you choose?
The models of these devices differ in the diameter of the particles created in the air suspension and in the principle of operation.
The size of microscopic droplets of a drug in an aerosol is called dispersion, and the higher it is (that is, the particle diameter is smaller), the deeper the drug can penetrate into the bronchial tree. When coughing (both dry, and wet, and wet), in order to select the desired dispersion of the nebulizer, you must first determine the cause that caused the appearance of the cough symptom, and therefore the level of damage to the respiratory tract.
- A finely dispersed aerosol penetrates into the narrowest and most distant parts of the bronchial tree. It is used for bronchiolitis and lesions directly to the lung tissue and alveoli.
- Medium-dispersed aerosol is used for bronchial inflammation of various calibers and bronchial asthma.
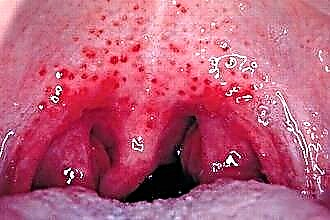
- Coarse aerosols usually do not penetrate deeply into the respiratory system, being deposited in its upper parts. The use of such nebulizers is indicated for tracheal inflammation, laryngitis and pharyngitis.
Modern models often allow you to adjust the dispersion of the generated air suspension. Thanks to this, it becomes possible to independently determine which part of the respiratory system should receive the main therapeutic effect during inhalation.

According to the mechanism of drug aerosol formation, nebulizers are subdivided into:
- Compressor rooms that create an air suspension of the drug by supplying it with an air stream under pressure.
- Ultrasonic, which mix and saturate the solution with air, acting on it with ultrasonic waves.
- Membrane, in which the liquid enters a special membrane that has a large number of holes on the surface - by vibrating, this membrane passes the drug through itself, turning it into an aerosol.
The choice of a nebulizer design depends on which drugs are planned to be administered by inhalation using this device.
Important! Each of the types of nebulizers has specific restrictions on the use of certain drugs, indicated below.
Mucolytic agents
 These drugs are the mainstay of inhaled cough treatment as a separate symptom. With a dry cough, the effect of such medicinal substances is primarily aimed at stimulating and enhancing the production of sputum by the walls of the bronchi. Thus, a painful, "tearing" dry cough will turn into a wet, productive cough.
These drugs are the mainstay of inhaled cough treatment as a separate symptom. With a dry cough, the effect of such medicinal substances is primarily aimed at stimulating and enhancing the production of sputum by the walls of the bronchi. Thus, a painful, "tearing" dry cough will turn into a wet, productive cough.
Inhalation with a wet cough can increase the production of mucus, make it less viscous and thick. In addition, mucolytics often simultaneously stimulate the motor function of the bronchi, that is, they contribute to the intensive excretion of sputum.
The most commonly used mucolytics are lazolvan and ambrobene, produced on the basis of abromcol, as well as ACC (Fluimucil), where acetylcysteine is the active ingredient.
These drugs are mainly sold in sealed spray bottles with dispensers. They are administered twice a day at the dose recommended by the doctor. If you use a personal nebulizer, an equal volume of saline must be added to the medication before refueling. Mucolytics are used in all types of nebulizers.
Bronchodilators
Inhalation of these drugs for coughing with a nebulizer is used if the pathology that caused the cough syndrome is associated with bronchial obstruction or spasmodic phenomena in the airways. Accordingly, before stimulating the formation and excretion of sputum, it is necessary to expand the lumen of the bronchial tube.
Bronchodilators such as Berodual, Berotek and Atrovent are administered through a nebulizer. These medicines are almost always sold in sealed spray bottles. When using the solution in a personal nebulizer, there are no restrictions on the design of the device.
Anti-inflammatory drugs
The cough is always accompanied by an inflammatory lesion of the mucous membrane of the respiratory tract. And non-steroidal drugs are used to relieve intense inflammation and alleviate the patient's condition. Since this is a symptomatic treatment, it is preferable to use agents that have several types of effects. An example is Cromohexal, which not only works as an anti-inflammatory, but also has a desensitizing effect.
 You can also fight inflammation with purchased phytopreparations, such as Rotokan - an extract of chamomile, medicinal calendula and yarrow. Before filling the nebulizer Rotokan must be diluted with saline in a ratio of 1 to 40. Non-steroidal agents can be used in any type of device.
You can also fight inflammation with purchased phytopreparations, such as Rotokan - an extract of chamomile, medicinal calendula and yarrow. Before filling the nebulizer Rotokan must be diluted with saline in a ratio of 1 to 40. Non-steroidal agents can be used in any type of device.
Hormonal drugs belonging to the class of glucocorticosteroids (GCS) also have an anti-inflammatory effect, but they are not used for a cold cough.
Their power is excessive to suppress the cough symptom in this case. But if the cough is caused by systemic, autoimmune lesions or is of an allergic nature, then the use of GCS is fully justified.
Glucocorticosteroids, as well as the antibiotics described below, cannot be used in ultrasonic nebulizers. Ultrasonic waves, passing through a liquid, heat it, and thermal effects destroy the molecular structure of these substances.
Antibiotics and antiseptics
Cough syndrome is almost always a consequence, a manifestation of another disease of the respiratory system. And in the overwhelming majority of cases, these are infectious lesions. Therefore, inhalations with antibiotics, although they do not cure the cough itself, but affect the cause of its occurrence. Having cured the underlying pathology, the patient will get rid of its symptoms, including any form of cough.
With the help of nebulizers, antibiotics such as gentamicin and Fluimucil-antibiotic IT are administered.
Antiseptic agents also destroy bacteria, but formally they do not belong to antibiotics, since they have a different origin. In nebulizers, these drugs are used without restrictions. It is recommended to inhale when coughing:
- chlorophyllipt solution;
- dioxidine solution;
- furacilin solution;
- purchased solution of calendula.
Mineral water and saline
 0.9% sodium chloride solution in water is closest to the natural environment of the body in terms of osmotic characteristics. Therefore, inhalations with saline will not harm the mucous membranes, providing them with moisture and softening. The same applies to mineralized waters such as Essentuki or Narzan. They are, of course, not a saline solution, but their input-salt balance is still very close to that of a human.
0.9% sodium chloride solution in water is closest to the natural environment of the body in terms of osmotic characteristics. Therefore, inhalations with saline will not harm the mucous membranes, providing them with moisture and softening. The same applies to mineralized waters such as Essentuki or Narzan. They are, of course, not a saline solution, but their input-salt balance is still very close to that of a human.
Inhalation with saline or mineral water is useful for both wet (dilution of sputum) and dry (removal of mucosal irritation) cough.
For one procedure, it is enough to pour 4-5 ml of liquid into the nebulizer without heating or diluting it.
These fluids are used in all types of nebulizers. Carbonated mineral waters are an exception - they cannot be inhaled with nebulizers.
Soda-salt solutions
Relief of a patient's condition with a persistent cough can be easily achieved by inhalation with baking soda and / or kitchen salt solutions. The optimal recipe includes diluted in 1 liter of water:
- 1 tablespoon of baking soda;
- 1 tablespoon salt
- 10 drops of iodine.
Such a mixture cannot be used in membrane nebulizers, because even with a very thorough dissolution of salt and soda, solid particles will still remain in the liquid that can damage the membrane or clog its holes. It is useful to replace kitchen salt with sea salt, but iodized salt is not applicable here - it irritates the mucous membrane.
Infusions and decoctions of phytopreparations
 Home-made solutions and herbal extracts are widely used for nebulizer inhalation for coughing. The limitation here is the impossibility of using such drugs in membrane nebulizers. It will not be possible to remove all solid components from the liquid even with the most thorough filtration. Here are some recipes for coughing:
Home-made solutions and herbal extracts are widely used for nebulizer inhalation for coughing. The limitation here is the impossibility of using such drugs in membrane nebulizers. It will not be possible to remove all solid components from the liquid even with the most thorough filtration. Here are some recipes for coughing:
- 1 teaspoon of mullein flowers and the same number of elderberry flowers in a glass of boiling water;
- take half a liter of boiling water in 1 teaspoon of thermopsis and 5 teaspoons of primrose herb;
- brew 10 teaspoons of dry coltsfoot in half a liter of boiling water, the same amount of rosemary and plantain;
- for half a liter of boiling water, take 5 teaspoons of pine buds and an equal volume of chamomile;
- antitussive collection includes sage, string, chamomile, eucalyptus, calendula and licorice rhizome - pour 2 teaspoons of the mixture with 200 g of boiling water.
All these solutions must be allowed to brew for at least 1 hour. Better if they cool on their own. Then strain the liquid through cheesecloth and fill it into a nebulizer.
Important! Medicinal herbs and oils can cause allergies. Make sure that the patient does not have an individual intolerance to the substances used for inhalation.
Vegetable oils
Essential and aromatic oils are excellent at softening the mucous membrane of the throat with a dry cough. In this case, it is recommended to inhale with lemon and eucalyptus oil. If the formation of phlegm in the respiratory tract has already begun, then the cough gradually becomes moist. To liquefy too thick and viscous mucus, and to stimulate bronchial motility, which enhances the evacuation of sputum, it is useful to inhale with aniseed and mint oil.
Remember that you can inhale essential and aromatic oils only with the use of some models of compressor nebulizers. To obtain a solution, you need to dilute 2-3 drops of oil in 1 liter of water. It is not recommended to mix oils and increase the dosage.