Purulent otitis media is an infectious ENT pathology that covers all parts of the middle ear: the mastoid process, the mucous membranes of the tympanic cavity and the Eustachian tube. Purulent inflammation is provoked by microbial microflora, which is represented mainly by cocci. Pathological processes in the ear cavity often cause the appearance of adhesions on the tympanic membrane, which leads to the development of hearing loss.
Causes

What is purulent otitis media? Ear pathology is characterized by catarrhal processes in the ear cavity, in which all parts of the middle ear are involved. The reason for its development is a decrease in the body's resistance, which entails the penetration and active reproduction of the bacterial flora. Through the Eustachian tube, microbial agents that saprophyte in the pharynx penetrate into the middle ear. But if the reactivity of the immune system is not reduced, inflammation does not occur.
In cases where the pathogenic microflora entering the ear departments is highly virulent, acute inflammation develops. In 80% of cases, the causative agents of infection are pneumococci, influenza, streptococci and Staphylococcus aureus. Bacteria and viruses penetrate into the corresponding parts of the ear cavity in a turbogenic way during the development of common infections, which include:
- flu;
- chronic rhinitis;
- sinusitis;
- pharyngitis;
- tuberculosis;
- scarlet fever;
- sore throat;
- pneumonia.
According to statistics, otitis media accounts for at least 30% of all ear pathologies. The disease is more susceptible to children under the age of 14 and the elderly with weakened immunity.
Is purulent otitis media contagious? Despite the fact that the pathology is infectious, it is almost impossible to become infected directly with otitis media. Ear disease is a complication that occurs against the background of general damage to the body by respiratory or microbial infections.
Pathogenesis
 Catarrhal processes always begin with damage to the mucous membrane of the Eustachian tube. Neutrophilic tissue infiltration occurs, resulting in severe edema of the auditory tube. Violation of its drainage function leads to the accumulation of exudative fluid in the tympanic cavity. Subsequently, the mucous membranes of the affected ear sections thicken, and the exudate becomes more viscous, which causes ulceration of the mucous membranes.
Catarrhal processes always begin with damage to the mucous membrane of the Eustachian tube. Neutrophilic tissue infiltration occurs, resulting in severe edema of the auditory tube. Violation of its drainage function leads to the accumulation of exudative fluid in the tympanic cavity. Subsequently, the mucous membranes of the affected ear sections thicken, and the exudate becomes more viscous, which causes ulceration of the mucous membranes.
With the progression of purulent otitis media, the tympanic cavity is filled with liquid contents and granulations. For this reason, deformation and protrusion of the tympanic membrane occurs. Continuous pressure of purulent masses on the membrane leads to its perforation, followed by otorrhea. With the cessation of suppuration, almost all symptoms of the disease subside, after which the integrity of the tympanic membrane is restored.
The spread of pus in the ear can lead to melting of the surrounding tissue, which is fraught with the appearance of adhesions to the tympanic membrane. This leads to a decrease in its elasticity and the development of hearing loss.
Clinical manifestations
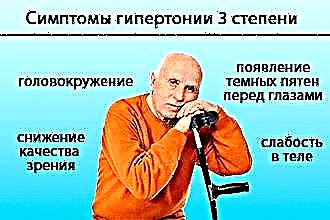
In most cases, ear pathology is characterized by a staged course, which facilitates the diagnosis process. In this case, the severity of local and general manifestations of the disease is determined by the severity of the development of catarrhal processes. The main symptoms of purulent otitis media in adults include:
- throbbing and aching pain in the ear;
- slight hearing impairment;
- headaches and malaise;
- ear congestion;
- audible hallucinations;
- hyperthermia.
In the course of ENT disease, there are three main stages in the development of purulent-catarrhal processes:
- preperforative - accompanied by an acute manifestation of the main symptoms of pathology: shooting pains, aggravated by palpation of the tragus, hyperthermia and hearing loss. Gradually, pus accumulates in the ears, as a result of which the eardrum protrudes outward;
- perforated - perforation of the tympanic membrane, followed by suppuration from the ear canal. In connection with the evacuation of purulent masses from the ear cavity, the clinical manifestations of pathology gradually subside;
- reparative - after the release of pus from the ear canal, epithelialization of tissues is observed, which leads to the restoration of the integrity of the tympanic membrane.

Acute otitis media
The main reason for the development of purulent otitis media is the reproduction of pathogenic microflora that penetrates into the ear canal from the nasopharynx. With the progression of pathological processes, the disease goes through the following stages of development:
- catarrhal - the formation of a liquid (serous) exudate in the middle ear, provoked by inflammation of the Eustachian tube. Destructive processes in the tissues lead to the radiation of pain in the teeth, back of the head, eyes, etc. This stage of development of purulent otitis media lasts from two days to two weeks;
- purulent - perforation of the tympanic membrane with further suppuration. As the purulent masses are evacuated, the pains dull and after 3-4 days they completely disappear;
- regressing - attenuation of purulent and catarrhal processes, accompanied by the regeneration of the tympanic membrane.
The development of suppurative otitis media of the middle ear increases the risk of hearing loss or deafness. Large perforations in the tympanic membrane are not tightened by connective tissue, but are closed by mucous masses. Salts are deposited on the atrophied area of tissue over time, which leads to a decrease in its elasticity. Often, adhesions from fibrous fibers also appear on the auditory ossicles, which leads to a restriction of their mobility.
With the development of purulent processes in the ear, you should seek the help of a specialist. Timely assistance of an ENT doctor will prevent degenerative changes in the mucous membranes of the main parts of the middle ear.
Chronic otitis media
Chronic otitis media is an ear pathology, accompanied by a recurrent course of catarrhal processes in the ear cavity. Persistent perforation of the tympanic membrane can cause severe hearing impairment and the development of autophony. In some cases, hearing loss is approximately 50-60%, which is fraught with the development of complete deafness.
Sluggish purulent otitis media in adults is a consequence of infectious rhinitis, pharyngitis, sinusitis, or inadequate treatment of other types of ear pathology. Possible intracranial complications arising from the development of the disease pose a great threat not only to health, but also to human life.
According to the results of bacterial culture, the main provocateurs of chronic inflammation are aerobic and anaerobic bacteria of the following types:
- pseudomonas;
- peptococci;
- lactobacilli;
- fusobacteria;
- pneumococci;
- staphylococci.
Depending on the localization of the perforated hole, chronic disease is conventionally divided into two types:
- mesotympanitis is a relatively mild form of pathology, characterized by purulent lesions of the mucous membranes in the ear cavity. The perforation in the membrane is located in the center, which contributes to the normal flow of pus from the ear;
- epitympanitis is a severe form of pathology, accompanied by the involvement of the mastoid bone tissue in catarrhal processes. Perforated holes are located in the upper sections of the membrane, in addition, they can cover its central part.
 This form of pathology is fraught with the development of very serious complications, which include sepsis, meningitis, osteitis, hydrocephalus.
This form of pathology is fraught with the development of very serious complications, which include sepsis, meningitis, osteitis, hydrocephalus.
Important! In cases where the ears begin to fester, one cannot resort to self-treatment. In particular, the use of dry heat can cause the spread of purulent masses deep into the meninges.
Bilateral otitis media
Bilateral purulent otitis media is a type of ENT disease characterized by inflammation of the soft tissues in the middle ear and the rapid spread of lesions to adjacent tissues. In the overwhelming majority of cases, patients are diagnosed with bilateral inflammation, which, with inadequate therapy, leads to the formation of purulent masses inside the ear cavity.
The key role in the development of bilateral purulent otitis media belongs to the structural features of the mucous membranes of the Eustachian tube. It is rather loose and thin, therefore, when pathogens penetrate, it quickly swells, increasing several times. As a result, there is a violation of the drainage function of the tube, which leads to the accumulation of liquid exudate in the middle ear.
Due to the accumulation of large volumes of pus in the ear in an adult, the ear membrane begins to stretch, which causes discomfort. To stop inflammation and trophic changes in tissues, antibiotic therapy is used. They kill the pathogenic aerobic and anaerobic bacteria, which prevents the accumulation of purulent masses in the middle ear.
Therapy
Pathology is treated on an outpatient basis in cases where there are no serious complications caused by the formation of pus in the ears of an adult. To eliminate inflammatory processes, pain syndrome and tissue edema, the following means of conservative treatment are used:
- antibiotics ("Levomycetin", "Azithromycin") - kill pathogenic microbes that have caused the development of catarrhal and purulent processes in the ear;
- vasoconstrictor drops (Galazolin, Sanorin) - reduce tissue edema, which helps to restore the drainage and ventilation function of the Eustachian tube;
- analgesics ("Diclofenac", "Paracetamol") - relieve the throbbing and aching pains provoked by the tension of the tympanic membrane and inflammation of the mucous membranes in the middle ear.
If the ear is festering, antibiotic therapy should not be interrupted. The minimum course of treatment should be 7-10 days.
Antibiotic overview
Systemic treatment of ENT disease involves the use of antibacterial drugs. They are able to destroy pathogenic bacteria that provoke inflammation, which leads to a regression of the clinical manifestations of ear pathology. In cases where pus flows from the ear, the following types of drugs should be included in the treatment regimen for the disease:
- "Amoxicillin" is a broad-spectrum antibacterial drug, the components of which are active against most aerobic bacteria. Has a pronounced antiphlogistic and antimycotic effect;
- "Spiramycin" is a drug with a bacteriostatic effect. It is used to eliminate the main symptoms of allergy provoked by the reaction of the affected tissues to the action of metabolites of pathogenic microflora;
- "Cefazolin" is a bactericidal drug, the components of which are active against gram-positive bacteria. Kills microorganisms capable of producing penicillinase, which provides effective antibacterial treatment of pathology at any stage of development;
- Ceftriaxone is a cephalosporin antibiotic that inhibits the synthesis of cell walls of pathogens, which prevents their development. Active against fungal microorganisms and anaerobic microbes.
Important! Premature cancellation of therapy can provoke a relapse of the disease, which is fraught with the transition of acute otitis media into a chronic form.
Therefore, when achieving positive therapeutic results about the advisability of stopping the drug intake, it is worth consulting with an ENT doctor.


 This form of pathology is fraught with the development of very serious complications, which include sepsis, meningitis, osteitis, hydrocephalus.
This form of pathology is fraught with the development of very serious complications, which include sepsis, meningitis, osteitis, hydrocephalus.