The human heart is the main pump of the body, which is anatomically represented by four cavity formations with internal connections. The left ventricle (LV) plays an important role in the work of the cardiovascular system, since a large hemodynamic circle begins from its cavity, saturating the entire body with oxygenated blood. To maintain an adequate supply of organs, the LV is characterized by a developed muscle layer and a more complex structure in comparison with the right "neighbor".
How does the left ventricle work?
 The left ventricle is a cavity formation. Its volume depends on the age of the person and the type of activity, since the muscles of the myocardium lend themselves to "training". The LV wall thickness is 10-14 mm and consists of three layers in which the fibers have different directions (circular, straight and oblique). Inside, the chamber is lined with an endocardium - a connective tissue sheath that forms the valves near the atrioventricular openings.
The left ventricle is a cavity formation. Its volume depends on the age of the person and the type of activity, since the muscles of the myocardium lend themselves to "training". The LV wall thickness is 10-14 mm and consists of three layers in which the fibers have different directions (circular, straight and oblique). Inside, the chamber is lined with an endocardium - a connective tissue sheath that forms the valves near the atrioventricular openings.
The shape of the left ventricle is oblong-oval, conical. There are two divisions of the structure:
- the top is a narrow part, which in a healthy person is located in the 4-5 intercostal space on the left;
- the outer edge is a rounded contour that forms the lateral (pulmonary) surface - the most massive part of the heart muscle.
Inside the LV consists of two parts: the posterior and anterior sections, along which the blood moves in stages from the chamber cavity to the aortic cone.
In the area of the atrioventricular opening, a valve is located, represented by two leaflets from the endocardial tissue. The main task of this structure is to regulate blood flow and prevent regurgitation (reflux). It is attached to the ventricular myocardium by papillary (papillary) muscles, the tone of which determines the amplitude of valve movement.
The aortic valve is represented by three semilunar flaps, which are attached around the circumference of the opening between the arterial cone and the aorta. The coordinated work of the valves ensures the movement of fluid into the systemic circulation during contraction of the LV myocardium and prevents regurgitation when the chamber is filled during diastole.
The wave of excitation, which causes the ventricle to contract, passes from the atrioventricular junction along the left bundle branch and its two branches. The cardiomyocytes located at the apex of the heart receive an impulse through the Purkinje fibers.
Main functions of the department
The left ventricle of the heart is responsible for the following functions:
- systolic - synchronous contraction of cardiomyocyte fibers provides adequate release into the systemic circulation to supply all organs and tissues with oxygen;
- diastolic - relaxation of the walls of the ventricle, opening of the atrioventricular valve and filling the cavity with blood from the atrium.
The normal pumping function is the well-coordinated work of all departments. The cardiac cycle consists of alternating states: systole and diastole, which are characterized by contraction and stretching of the muscle fibers of cardiomyocytes.
Systolic phase periods:
- voltage with a stage of asynchronous and isometric contraction;
- expulsion (two periods - fast and slow).
The asynchronous period is characterized by an uneven distribution of the excitation pulse, therefore, individual fibers do not contract simultaneously. A similar phase is necessary for the complete closure of the mitral valve leaflets, after which intraventricular pressure increases (due to the continued contraction of cardiomyocytes). Having reached the level of 70-80 mm Hg. Art., the semilunar valves open and blood enters the aorta (first quickly, and then more slowly). The closing of the valve is due to the high pressure inside the vessel.
Relaxation of the myocardial wall of the LV opens the mitral valve, which starts the flow of a new portion of blood. To ensure adequate ejection, it is necessary that all parts of the ventricle, cusps, papillary muscles, trabeculae and chords are in good functional condition.
Disease Diagnostics: What Methods Will Determine the Problem?
There are two types of left ventricular dysfunction (dysfunction):
- Systolic, which is characterized by a drop in the ejection capacity of the LV. Most often, pathology develops when contractile cardiomyocytes are damaged during myocardial infarction, inflammatory or autoimmune disorders.
- Diastolic. It is characterized by the inability of muscle fibers to completely relax and create the required volume of the chamber (the condition is diagnosed most often with pathologies of the pericardium or adjacent structures).
If there are complaints of shortness of breath during exercise or at rest, swelling in the legs, cough, pain in the heart area, you should contact a cardiologist and undergo a comprehensive examination to find out the cause.
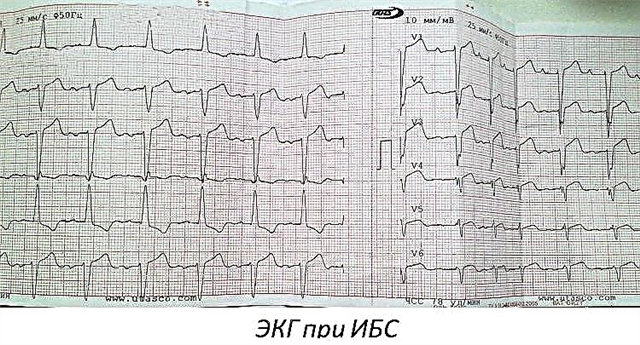
ECG
With the help of electrocardiography (ECG), it is possible to reveal not only the correctness of the rhythm, heart rate, but also disturbances in the work and structure of the left ventricle. Signs of ECG changes in various LV pathologies:
- Hypertrophic changes in the walls of the left ventricle, regardless of the reasons:
- displacement of the electrical axis of the heart to the left (angle α is from -90 to 0 °);
- intraventricular conduction disturbances (complete or incomplete left bundle branch block);
- repolarization disorders - deformation of the T wave in I, aVL, V5, V6.
- Cicatricial phenomena in the left ventricle:
- altered Q wave in I, II, aVL-leads, as well as in V1-6;
- location of ST on the isoline;
- low and smoothed T wave.

Ultrasound
Ultrasound or echocardiography (echocardiography) helps to determine the size of the heart chambers and the thickness of their walls, to assess the functional state of the valves, the effectiveness of myocardial contraction. Each department has its own norm indicators.
The main ultrasound parameters of the LV are presented in the table.
| Criterion | Standards | Changes |
|---|---|---|
| Muscle mass |
| Increase - with hypertrophy (distinguish symmetric and asymmetric growth) |
| Myocardial mass index (LVMI) |
| |
| Ventricular septum thickness (IVS) |
|
|
| End diastolic volume (EDV) |
| |
| Final size |
| |
| Ejection fraction (EF) | 55-60% | A decrease in the indicator is characteristic of systolic dysfunction of the left ventricle. |
| Stroke volume (SV) | 60-100 ml |
|
Scintigraphy
Perfusion scintigraphy is a method of assessing the blood supply to the muscle layer of the left ventricle using radiopharmaceuticals that are administered intravenously, and they accumulate in the myocardium. The advantage of the study is the accurate detection of ischemia even in small vessels, which is not always possible to detect with angiography. Scintigraphy can be static (performed at rest) and dynamic (during dosed exercise on a bicycle ergometer).
Indications for conducting:
- myocardial ischemia of undetermined origin;
- assessment of the effectiveness of operations to restore coronary blood flow (angioplasty, bypass surgery, etc.);
- studies of myocardial blood flow in non-coronary diseases (mainly of an inflammatory nature);
- with questionable ECG (to confirm the diagnosis of acute myocardial infarction).
MRI and CT
Recently, X-ray methods for examining the heart have been in demand, which make it possible to obtain volumetric images of an organ and reveal changes in the structure.
A computed tomography (CT) scan takes a series of x-rays of the heart from different angles on separate sections of the organ. Modern devices are capable of providing three-dimensional visualization of the internal structure.
Magnetic resonance imaging (MRI) has a similar principle. However, the study does not use ionizing radiation, but magnetic waves. Tissues differently "respond" to this effect, which is recorded by the apparatus.
Both methods can provide information like this:
- LV wall thickness;
- changes due to myocardial infarction;
- vascular condition, the presence of atherosclerotic plaques;
- the adequacy of hemodynamics;
- condition of the pulmonary arteries.
What pathologies most often affect the work and structure of the LV?
There are many pathological conditions and provoking factors that lead to changes in the anatomical structure and physiological dysfunction of the left ventricle. In some cases, LV hypertrophy is a normal variant, for example, in athletes or pregnant women.
Pathologies that are accompanied by a violation of the left ventricle:
- congenital defects: coarctation of the aorta, anomaly of the interventricular septum, combined disorders - tetrad or pentad of Fallot;
- inflammatory diseases: endo-, myo-, pericarditis (children and adolescents are more often influenced);
- acquired heart defects (more often diagnosed in adults as a consequence of rheumatism);
- IHD: angina pectoris, postinfarction cardiosclerosis, myocardial wall necrosis;
- chronic lung disease;
- arterial hypertension;
- atherosclerosis of the aorta;
- the consequences of metabolic syndrome in combination with obesity and diabetes mellitus;
- pathology of the kidneys, liver, thyroid gland.
Without adequate treatment and correction of hemodynamics, the patient's condition worsens: heart failure progresses, the brain and all internal organs experience oxygen starvation.
At the first manifestations of left ventricular dysfunction, it is recommended to visit a therapist (cardiologist), undergo examinations to prevent further development of pathology. Patient management depends on the underlying disease and involves the use of pharmacological drugs or cardiac surgery.
Adjunctive therapy includes lifestyle modification, compensation for associated disorders.
Conclusions
Of all parts of the heart, the left ventricle plays the greatest role in ensuring adequate blood circulation. Large chamber volume, thick muscular wall and aortic outlet are key characteristics that determine the importance of structure. The defeat of the LV by ischemic, traumatic, inflammatory processes is accompanied by severe hemodynamic defects with symptoms of heart failure. Shortness of breath, edema, chest pain, a feeling of interruptions in the work of an organ are signs of serious disorders that require comprehensive diagnosis and adequate therapy.