Acute myocardial infarction is a serious pathology. Timely help and adequate therapy affect the future prognosis for a person. The quality and duration of life after a heart attack depends on many factors. Instrumental diagnostics and a detailed survey of the patient will help to make a prognosis for each specific case. You can influence the development of the disease with the help of drug therapy and lifestyle changes.
How a heart attack affects the quality and duration of life
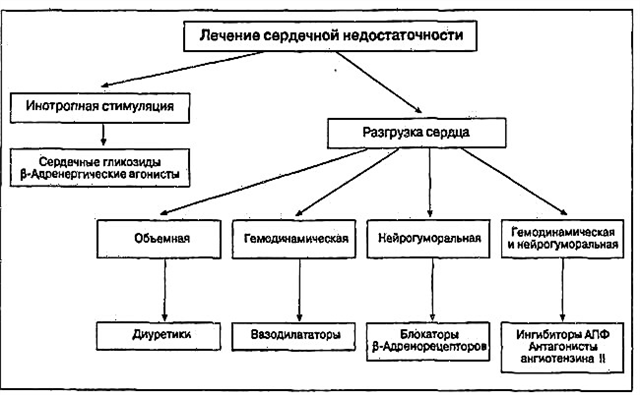
Myocardial infarction is considered an acute form of coronary heart disease (IHD), which is characterized by impaired blood supply to muscle fibers and the development of necrosis with scar formation. Dense connective tissue does not perform the necessary contractile and conductive function, which contributes to the development of heart failure. Violation of blood circulation worsens the patient's quality of life and often becomes the cause of disability.
Factors affecting the general condition of the patient after myocardial infarction:
- severe swelling in the legs, accumulation of fluid in the abdominal and chest cavity with the development of shortness of breath;
- recurrent chest pain (usually at night);
- constant fatigue;
- sleep disturbance;
- the need to limit the usual physical activity;
- complete cessation of alcohol and smoking;
- change in diet;
- difficulties in sexual life;
- travel and travel restrictions;
- addiction to drugs and frequent side effects;
- material costs associated with the purchase of medicines.
An objective assessment of the impact of myocardial infarction (MI) on a person's life is carried out using special scales and standardized questionnaires.
Statistics
The introduction of surgical interventions (shunting and stenting) into clinical practice is encouraging: the incidence of complications in the early period has decreased over the past 15 years by 25%. The most common causes of death after a heart attack are:
- acute heart failure with the development of pulmonary edema;
- cardiogenic shock - a systemic circulatory disorder with a drop in blood pressure;
- acute aneurysm of the left ventricle - thinning of the wall with protrusion. Its rupture is accompanied by cardiac tamponade: the cavities of the pericardium are filled with blood, disrupting the contractile function of the myocardium;
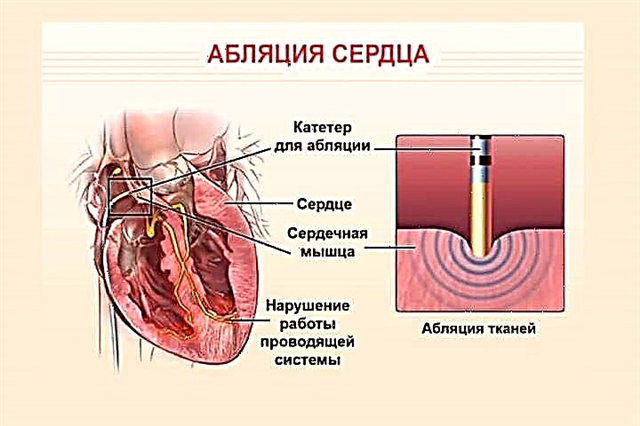
- rhythm and conduction disturbances (ventricular or atrial fibrillation, complete atrioventricular block, and others);
- systemic thromboembolism - the spread of blood clots throughout the vascular bed with blockage of the arteries of the kidneys, brain (with the development of a stroke);
- recurrence of a heart attack.
How long do patients live on average?
The prognosis for myocardial infarction depends on the characteristics of the course of the pathology and other factors, including age, gender, the presence of concomitant diseases. The timeliness of the assistance provided and the systemic intake of medications (before an acute coronary event) also affect the outcome of the pathology.
Life expectancy statistics after myocardial infarction are presented in the table.
| The period after discharge from the hospital | Percentage of people who live after a heart attack |
|---|---|
| 1 year | 80% |
| 5 years | 75% |
| 10 years | 50% |
| 20 years | 25% |
In medical practice, there is an opinion that 25% of all deaths from a heart attack occur in the first minutes, 50% - in the first hour, 75% - on the first day. The absence of acute complications within 24 hours is the key to a favorable prognosis for the patient.
What determines the duration of the life ahead?
How long and how you can live after a heart attack are determined by the following indicators:
 Q wave on the electrocardiogram (characterizes the presence, localization and size of the scar in the myocardium);
Q wave on the electrocardiogram (characterizes the presence, localization and size of the scar in the myocardium);- spread of the process: extensive (transmural) infarction has a more unfavorable prognosis in comparison with large focal;
- arterial hypertension - a persistent increase in blood pressure;
- diabetes mellitus and the degree of its compensation;
- smoking and drinking alcohol;
- violation of lipid metabolism with an increase in cholesterol, low-density lipoprotein;
- dysfunction of the left ventricle;
- the formation of heart failure;
- the presence of arrhythmias (atrial fibrillation, high-grade extrasystole, atrioventricular blockade, and others);
- timeliness of assistance - thrombolytic therapy or reperfusion (restoring blood flow) operations.
The statistical characteristics of the 3-year survival rate of patients with acute myocardial infarction are presented in the table.
| Indicator | Survival |
|---|---|
| Pathology form |
|
| Floor |
|
| Age |
|
What is the prognosis of a patient with a heart attack and how to influence it
The general prognosis in the postinfarction period is calculated separately for each patient, since additional data on the comorbid background and individual characteristics are taken into account.
Modern methods of diagnosis and emergency care increase the survival rate after a heart attack by up to 90% within the first year.
 To improve the prognosis on their own, patients are advised to:
To improve the prognosis on their own, patients are advised to:
- monitoring the course of the disease with regular examinations and additional studies;
- see a doctor when new symptoms appear;
- lifestyle change;
- systemic medication (for the treatment of hypertension, arrhythmias, prevention of lipid disorders and thrombus formation).
After suffering myocardial infarction, lifelong treatment and rehabilitation is required in order to prevent complications and the development of pathologies in other organs and systems.
Correction of risk factors
The death of a patient in the early or late post-infarction period is largely determined by the risk factors for the development of complications or recurrent myocardial infarction.
In order to prevent and increase life expectancy, it is recommended:
- lifestyle modification: adequate physical activity, rejection of bad habits and good nutrition;
- normalization of weight using non-drug methods. If ineffective, pharmacological agents are prescribed;
- monitoring blood pressure indicators;
- avoidance of stressful situations;
- systemic intake of prescribed drugs.
Treatment of concomitant pathology
 Injuries, infectious and endocrine diseases aggravate the course of coronary heart disease, therefore control and adequate therapy of concomitant pathologies affects the prognosis for the patient. Mandatory correction is required:
Injuries, infectious and endocrine diseases aggravate the course of coronary heart disease, therefore control and adequate therapy of concomitant pathologies affects the prognosis for the patient. Mandatory correction is required:
- diabetes mellitus - glucose monitoring is carried out in a cardiological hospital to take into account the risk of complications and prescribe treatment;
- myocarditis - inflammation of the muscle mass of the heart worsens the course of the postinfarction period with the development of rhythm disturbances, a decrease in contractile function;
- kidney disease - impaired excretion of fluid from the body, disorders of hormone synthesis lead to damage to the vascular wall, increased blood pressure;
- pathology of the thyroid gland (Hashimoto's goiter, diffuse toxic goiter and others).
Traumatic brain injuries with damage to the medulla oblongata (this is where the center for the regulation of vascular tone and cardiac activity is located) worsen the prognosis of rehabilitation after a heart attack.
Conclusions
The death of a part of the heart muscle is always accompanied by generalized disorders throughout the body. The quality of medical care significantly affects the prognosis of postinfarction patients.Subject to the recommendations and careful attention to health, the patient can live a long full life after a heart attack.

 Q wave on the electrocardiogram (characterizes the presence, localization and size of the scar in the myocardium);
Q wave on the electrocardiogram (characterizes the presence, localization and size of the scar in the myocardium);