The supply of the blood volume necessary for the body is ensured by the well-coordinated work of the cardiac muscle sections. The contraction of the system of cavities connected by holes promotes alternate emptying and filling of the atria and ventricles. The heart is located between the vessels of the lungs (where the blood is saturated with oxygen) and the arteries that feed the rest of the human body.
The heart cavity includes the ventricles and atria. They are separated by valves: tricuspid (consists of three valves) on the right and mitral (MK, bicuspid) on the left.
Why is there a reverse flow of blood into the MC?
The pumping function of the heart is provided by the left ventricle. When he relaxes, the blood from the atrium through the mitral opening flows into his cavity. This is the diastole phase. During systole, the ventricle contracts, pushing the blood contained in it into the vascular bed.
Tightly closed fibrous plates - the leaflets of the mitral valve - prevent blood from flowing back into the atrium. If their edges do not touch during systole, part of the fluid volume moves back, and regurgitation occurs.
This condition is called mitral regurgitation.
Degenerative processes in the valves can be the reasons for the reverse flow of blood. Changing the structure of the valve disturbs the shape of its edges and negatively affects the range of motion.
- systemic lesions of the connective tissue (for example, scleroderma);
- congenital hereditary diseases (Ehlers-Danlos syndrome);
- rheumatism;
- endocarditis of infectious etiology;
- rupture of chords (thin strings that connect the edge of the valve and the bottom of the left ventricle; the main function is to prevent eversion (prolapse) of the leaflets towards the atrium);
- dysfunction of the papillary muscles (located at the base of the chords);
Valvular mitral regurgitation can be caused by a change in the myocardium with a normal valve structure:
- expansion of the mitral ring;
- pathological enlargement of the left ventricular cavity (with heart failure);
- hypertrophic cardiomyopathy (characteristic of hypertension stages 2, 3).
The atrioventricular opening is rounded. The basis for the valves is the annulus fibrosus welded to the myocardium. If the heart muscle is stretched, the shape of the hole will change.. In this case, the unchanged valves will not be able to perform their function (tightly block this outlet for blood during systole) and regurgitation will occur.
If the bicuspid valve does not close completely, this triggers a cascade of pathological processes:
The return of a part of the blood volume to the left atrium causes stretching of its walls (dilatation) and blood overflow.
- The myocardium has to push out a larger volume, the muscle fibers are hypertrophied compensatory, contract more strongly.
- Since blood in the left atrium comes from the pulmonary circulation, the pressure in the lungs rises (here the first characteristic symptom arises - shortness of breath).
- The right ventricle pumps blood into the lungs, and to overcome the increased resistance, it also hypertrophies, but to a lesser extent.
- The left ventricle is gradually stretched by the increased incoming blood volume.
As long as he is able to cope with the increased load, there will be no clinical symptoms.
Process diagnostics and details of complaints
The disease can be diagnosed only after the patient seeks help. Mitral valve regurgitation of the 1st degree (up to 5 ml) is not clinically apparent. Symptoms arise already with a more significant violation of hemodynamics.
Long-term concealment of mitral insufficiency is provided by thickening of the left ventricular myocardium. However, when the reserves of this mechanism are depleted, the patient's condition deteriorates sharply.
There are 5 stages of mitral regurgitation.
| Stage | Complaints | Hemodynamic disorders | Treatment |
|---|---|---|---|
| Compensation | Absent | Clinically insignificant regurgitation, up to 1+ (no more than 5 ml) | Not required |
| Subcompensation | Shortness of breath when walking long distances, running | Regurgitation within 2+ (about 10 ml). Left heart: ventricular hypertrophy, atrial dilatation | Surgical treatment is not indicated |
| Right ventricular decompensation | Breathing problems with little exercise | Significant regurgitation, 3+. Dilation of the left ventricle, enlargement of the right sections. | Surgical treatments are recommended |
| Dystrophic | Shortness of breath without external causes, cough, edema, fatigue | Deterioration of the pumping function of the heart, relative insufficiency of the tricuspid valve | Surgical treatment indicated |
| Terminal | The patient's condition is grave. Hemoptysis, cough, edema, poorly healing ulcers. | Decompensation of the circulatory system | Treatment not indicated |
The army will not accept a person with regurgitation of the second degree or higher for military service!
Typical complaints in mitral regurgitation:
shortness of breath (first with significant physical activity, in the terminal stages - on an ongoing basis);
- palpitations (with physical activity);
- acrocyanosis (blue tips of the fingers);
- "Mitral butterfly" (bluish blush on the cheeks);
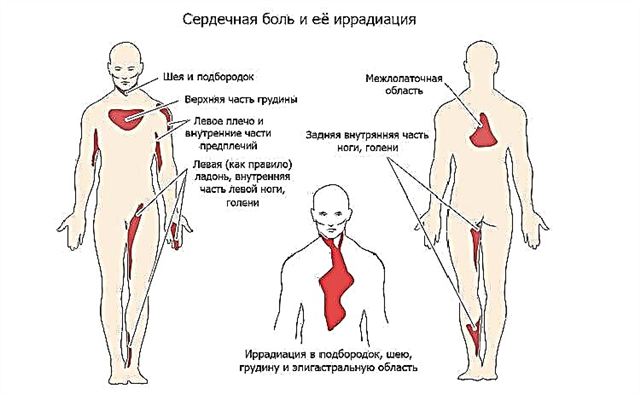
- cardialgia (pain in the heart, aching or pressing, sometimes stabbing, not necessarily associated with stress);
- edema on the legs (appear in the afternoon, in the evening, in the initial stages disappear overnight);
- pain in the right hypochondrium (appears as a result of blood stagnation, with pronounced edema);
- cough (with stagnation of blood in the pulmonary circulation, often unproductive);
- hemoptysis (with decompensation of the patient's condition).
Hemodynamic disorders can be diagnosed by such instrumental methods:
- electrocardiography (left ventricular hypertrophy, arrhythmias, after the third stage - right ventricular hypertrophy);
- phonocardiography (the first tone is weakened, systolic murmur is determined at the apex of the heart);
- echocardiography (enlargement of the heart cavities and thickening of the myocardium, changes in the movements of the interventricular septum, calcifications in the leaflets of the mitral valve);
- Doppler echocardiography (detection of the return of part of the blood to the atrium during ventricular systole).
Patient correction and recovery methods
Types of surgical interventions:
the imposition of clips and rings (correction of the shape of the leaflets and the width of the fibrous base of the valve);
- placement of a prosthesis (complete replacement of the mitral valve).
Principles of patient recovery after surgery:
- blood rheology support (thinning drugs);
- prevention of blood clots (antiplatelet agents);
- exclusion of significant physical exertion;
- long-term dispensary observation.
Conclusions
Regurgitation in the bicuspid valve occurs due to the inability of its cusps to close tightly during systole. The danger of reverse blood flow is the expansion of the cavities of the heart and their excessive filling with blood. To support the pumping function, the myocardium is compensatory hypertrophied. The heart muscle is not adapted for prolonged loads of this degree, therefore, decompensation occurs, expressed in characteristic clinical symptoms, the earliest of which is shortness of breath.
The gold standard for diagnosing regurgitation is Doppler ultrasound of the heart. Stage 3 and 4 of mitral regurgitation are subject to surgical treatment.