Aortic aneurysm is a severe organic pathology, which implies a defective expansion of the lumen of a specific section of a given vessel. Such changes lead to abnormalities in hemodynamics and progression of heart failure and other consequences. The disease can be congenital and acquired. A quarter of all cases are thoracic aortic aneurysms.
What is an aortic aneurysm?
An aneurysm is called an increase in the lumen of a vessel by more than 2 times in a limited area due to its thinning or stretching. In this case, protrusions or pockets are formed, as a result of which blood flow is disturbed. Usually, pathology occurs due to an abnormal process in the connective tissue. In this case, the inner part of the wall becomes thinner, under the high pressure of blood it stretches and begins to protrude. Over time, this phenomenon progresses and the aneurysm increases.
The aorta is one of the main blood vessels in humans, providing oxygenated blood to almost all organs. Also, the expansion of the aortic root (especially the Valsava sinus) can lead to compression of the coronary arteries supplying the heart muscle, which often results in the development of coronary artery disease. One of the most dangerous complications of aortic aneurysm is its rupture, which leads to sudden death.
There are three main forms of thoracic aortic aneurysm:
- saccular (the wall protrudes slightly in a small area);
- exfoliating (formed as a result of tearing of the intima);
- fusiform (the aorta of the heart is expanded around the entire circumference).
Causes of occurrence
Congenital causes primarily include genetic diseases of the connective tissue:
Marfan syndrome;
- Ehlers-Danlos syndrome;
- Erdheim's disease;
- congenital elastin deficiency.
However, most often this pathology has an acquired character - due to metabolic disorders, infectious, inflammatory, autoimmune diseases or injuries:
- atherosclerosis;
- aortitis due to bacterial or fungal diseases (sepsis, pneumonia, tuberculosis, syphilis, pericarditis);
- autoimmune diseases of connective tissue (Wegener's granulomatosis, Takayasu's arteritis, giant cell arteritis);
- mechanical damage (for example, in an accident or as a result of surgery).
There are also many risk factors that significantly increase the risk of this disease:
- age (more often elderly, from 55-60 years old);
- gender (5 times more often in men);
- arterial hypertension;
- alcohol abuse and smoking;
- obesity;
- hypodynamia;
- hypercholesterolemia, hyperlipidemia.
Typical and atypical clinical manifestations
In accordance with the nature of the flow, the following stages are distinguished:
Acute - occurs instantly in 2-3 days as a result of a heart attack or a massive inflammatory process. Very quickly ends in rupture, therefore requires immediate treatment;
- Subacute - most often it is a consequence of brought heart diseases or operations in the mediastinum, as a result of which scars are formed. Develops over several months;
- Chronic - is formed over a long period of time and is characterized by a high degree of compensation, which is why the clinic is unexpressed.
As practice shows, at the initial stages, this disease almost does not manifest itself, and its symptoms are too nonspecific, which is why they are detected only at the pre-rupture stage. All this greatly complicates early diagnosis.
The most pronounced symptoms are the expansion of the ascending part, arch and thoracic aorta, which is associated with their anatomical location.
In this case, protrusions can squeeze the organs of the mediastinum, which leads to the following manifestations:
- dry cough and shortness of breath (bronchi and trachea);
- Difficulty swallowing (esophagus)
- bradycardia (vagus nerve);
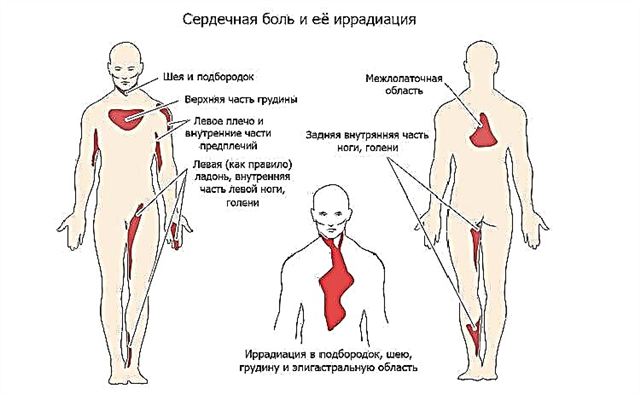
- chest pain (sensory nerves);
- frequent pneumonia, edema (root of the lungs).
The descending part of the thoracic aorta can compress the sympathetic plexus, intercostal nerves, which leads to the development of neuralgia and paresis. When the vertebrae are compressed, their deformations occur, the curvature of the spine.
It often happens that the disease manifests itself only during dissection and rupture of the aorta. In this case, the following symptoms and syndromes may occur:
- motor restlessness;
- weakness, shortness of breath, sweating;
- cyanosis;
- hoarseness of voice;
- fainting.
On examination, the asymmetry of the pulse is observed, the pressure drops (it may not be determined at all).
With delamination, the following complications can also occur:
- hemorrhagic shock;
- acute heart failure;
- hemothorax;
- hemopericardium (cardiac tamponade);
- stroke.
Diagnosis and differentiation of symptoms
Further examination includes the following methods:
X-ray of the OGK with contrasting of the esophagus;
- X-ray of the abdominal organs;
- echocardiography;
- ultrasound dopplerography of the thoracic aorta;
- CT or MRI;
- aortography.
Differential diagnosis is also very important, since many diseases manifest themselves in a similar clinic. The differential diagnosis of aneurysm of the thoracic aorta is carried out with:
- tumors of the mediastinum and lungs;
- cysts and neoplasms of the pericardium;
- congenital tortuosity of the aorta;
- intramural hematoma.
Treatment methods
For small aneurysms (especially congenital), expectant tactics can be used. The patient is shown periodic observation by a cardiologist and supportive therapy aimed at strengthening the walls of blood vessels. Anticoagulants, antihypertensive drugs, and statins are prescribed.
However, most often, due to the high likelihood of complications, surgical treatment is indicated.
The indications for surgery will be:
- the diameter of the defect is more than 5 cm;
- rapid increase in size;
- dissection of aneurysm
- traumatic etiology.
There are two main options - open and endovascular surgery.
The first technique - resection of the aortic aneurysm, is applied using an open-heart heart-lung machine. In this case, the damaged sections of the vessel wall are excised and then suturing is performed. In some cases, prosthetics with an implant is indicated.
It is preferable to use the second option as less traumatic, however, it is indicated only for small aneurysms in a place convenient for access.
The operation is performed as follows. A catheter is inserted through the femoral artery, in which a probe with a vascular prosthesis is placed. As soon as it approaches the aneurysmal site, it is fixed just above and below the expansion. In this case, all the blood begins to pass through the artificial tube.
After the intervention, the patient is transferred to the intensive care unit and drugs are prescribed to prevent thrombosis and infectious complications.
Conclusions
Aortic aneurysm is a statistically significant cause of death in the structure of cardiopathologies.
Symptoms of enlargement of the aorta of the heart are very nonspecific, due to which the detection of the disease occurs in the later stages. Even with the use of modern techniques, the operating mortality rate is 15-20%. The general prognosis for patients is unfavorable, however, proper rehabilitation and prevention significantly improves the quality of life.