Arrhythmias are violations of the regularity and frequency of the heartbeat. They cause more than just unpleasant sensations: some of the disorders significantly impair the quality of life and affect its duration. To help cope with this, medicine has invented antiarrhythmic drugs.
What arrhythmias should be treated and when?
There are such groups of changes in heart rate:
- Violation of automatism:
- sinus tachycardia;
- sinus bradycardia;
- sinus arrhythmia;
- sick sinus syndrome;
- rhythm from the lower atrium, atrioventricular node, ventricles.
- Pathology of excitability:
- extrasystoles;
- paroxysmal tachycardia.
- Conduction defect:
- Wolff-Parkinson-White syndrome;
- Clerk-Levi-Cristesco syndrome;
- blockade.
- Mixed pathologies:
- flutter and atrial fibrillation.
Not all of the above options require drug therapy. Treatment of arrhythmias with drugs can be considered for frequent episodes of this nature:
- pulse more often than 90 beats per minute;
- a feeling of trembling or fluttering in the chest;
- dyspnea;
- light-headedness;
- episodes of short-term loss of consciousness;
- pain in the region of the heart at the time of rapid rhythm.
When determining such symptoms, do not self-medicate - consult a cardiologist for advice.
How is drug treatment carried out?
In the practice of cardiologists and therapists, the international classification of antiarrhythmic drugs by class and generation is often used. So, there are four types, which are presented in the list of drugs for cardiac arrhythmias by name. Membrane stabilizers of the first class are divided into groups I a, I b and I c, depending on their type of exposure. Group Ia and Ic drugs affect sodium ion channels, Ib - potassium. The second class is beta-adrenergic blockers. Third - lengthening and slowing down the passage of the potential, blocking the flow of potassium ions through the membranes. Fourth - antiarrhythmics, which affect the calcium flow in the heart muscles. Fifth - combines other medicines with a similar effect. According to the division, the following are used in treatment:
- Class I:
- I a - "Quinidine", "Procainamide", "Disopyramide", "Aimaline";
- I b - "Lidocaine", "Meksilitin", "Trimekain", "Difenin";
- I with - "Flecainide", "Propafenone", "Etatsizin", "Allapinin".
- Class II: Propranolol, Metoprolol, Bisoprolol, Esmolol, Atenolol, Anaprilin.
- Grade III: Amiodarone, Sotanolol, Dofetilide, Azimilid, Bretilium.
- IV class. Verapamil, Diltiazem.
- Class V: "Digoxin", "Magnesium sulfate", "Potassium chloride", "Adenosine triphosphate".
Mechanism of action and pharmacodynamics of drugs
The normal sinus rhythm of the heart is disturbed by changes in excitability, automatism, conduction or formation of impulses along the myocardium. The principle of action of drugs for arrhythmia is a pronounced effect on the transfer of ions and electrical potentials of cardiomyocytes (muscle cells of the heart). This allows you to normalize the frequency and strength of contractions with medication without surgery or the installation of a pacemaker. Depending on the class and group, drugs have the following effect:
- stabilize the membranes of cardiomyocytes and act on sodium and potassium channels;
- affect adrenergic receptors and the sympathetic nervous system;
- block the current in the membranes of the heart cells.
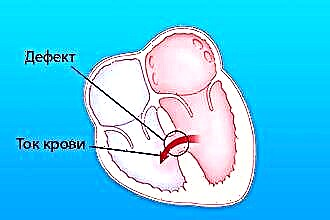
In the wall of each muscle cell of the heart, there are many channels through which ions of potassium, sodium, calcium and chlorine enter. When the particles move, an action potential is formed, and the impulses propagate along the conducting system. This process ensures contractility in the correct rhythm. With arrhythmias, nerve impulses pass abnormally. This happens as a result of new foci of activity, or when the current wanders in the wrong direction. Arrhythmia medications prevent this. Let's consider in more detail each of the classes and the characteristics of its representatives.
Sodium channel blockers
These drugs can block sodium from entering the cell. They slow down the passage of the excitation wave through the myocardium, which can lead to the termination of arrhythmia.
Effects:
- oppression of the sinus node and other pacemakers;
- decrease in myocardial excitability;
- decrease in the rate of excitation;
- lowering blood pressure;
- decrease in minute blood volume.
Within the class, subclasses are distinguished based on the properties of drugs to influence different types of arrhythmias. For example, some of the medications are better at dealing with supraventricular rhythm disturbances, others with ventricular arrhythmias.
І А class
This group includes drugs that have a membrane stabilizing effect: Novocainamide, Quinidine, Aimalin.
"Quinidine" - alkaloid. They get it from the bark of the cinchona tree.
Indications:
- ventricular and supraventricular tachycardias;
- atrial fibrillation;
- extrasystole;
- prevention of attacks of paroxysmal tachycardia.
Contraindications:
- heart failure;
- active inflammatory process in the myocardium;
- complete atrioventricular block;
- thrombus in the atrial cavities;
- pregnancy;
- atrial fibrillation due to thyrotoxicosis.
Side effects:
- dyspepsia;
- dizziness;
- hearing impairment, vision;
- arterial hypotension;
- heart failure;
- atrioventricular block;
- thrombocytopenic purpura.
"Novocainamide" - a synthetic derivative of novocaine.
 Indications:
Indications:
- paroxysmal ventricular and supraventricular tachycardia;
- atrial fibrillation;
- atrial flutter;
- ventricular premature beats.
Contraindications:
- heart failure;
- arterial hypotension;
- atrioventricular block;
- impaired liver and kidney function;
- parkinsonism.
Side effects:
- allergic reactions;
- nausea;
- vomit;
- insomnia;
- excitation;
- headache;
- convulsions;
- arterial hypotension;
- violation of the conduction of the heart muscle;
- flutter of the ventricles.
"Aymalin" Is a rauwolfia alkaloid.
Indications:
- ventricular arrhythmia in patients with myocardial infarction;
- Wolff-Parkinson-White syndrome.
Contraindications:
- severe conduction disturbances;
- myocarditis;
- circulatory insufficiency of the III degree;
- arterial hypotension.
Side effect:
- general weakness;
- nausea;
- vomit;
- arterial hypotension;
- feeling of heat.
І В class
This class includes: "Lidocaine", "Trimekain", "Mexiletin".
Their difference is that they have little effect on the sinus node, atria and atrioventricular junction, therefore, with supraventricular arrhythmias, they do not give the desired effect, but ventricular tachycardias and extrasystoles are removed excellently. Also, these pills for arrhythmia perfectly cope with disorders that arise as a result of an overdose of cardiac glycosides.
The brightest representative of the group - "Lidocaine".
Indications:
- ventricular premature beats;
- ventricular tachycardia;
- prevention of ventricular fibrillation, especially in the acute period of myocardial infarction;
- glycosidic intoxication;
- anesthesia.
Contraindications:
- epilepsy;
- allergy to lidocaine;
- sick sinus syndrome;
- bradycardia;
- cardiogenic shock;
- atrioventricular blockade I-III degree;
- glaucoma.
Side effects:
- psychomotor agitation;
- dizziness;
- convulsions;
- impaired vision and speech;
- collapse;
- allergy.
І С class
Includes Etatsizin, Flecainide, Propafenone (trade name Ritmonorm).
Members of this subclass have a strong antiarrhythmic effect. They are also able to provoke arrhythmias themselves (proarrhythmic effect) in some patients with myocardial infarction or heart failure.
"Propafenone"
 Indications:
Indications:
- prevention and treatment of ventricular premature beats;
- atrial fibrillation;
- supraventricular tachycardia;
- Wolff-Parkinson-White syndrome;
- Clerk-Levi-Cristesco syndrome.
Contraindications:
- heart failure;
- cardiogenic shock;
- sinus bradycardia;
- weakness of the sinus node;
- arterial hypotension;
- violation of cardiac conduction;
- myasthenia gravis;
- bronchospasm;
- obstructive pulmonary disease.
Side effects:
- nausea;
- vomit;
- gastroenteritis;
- constipation;
- dizziness;
- insomnia;
- bronchospasm;
- anemia;
- leukopenia.
Beta-blockers
Many diseases are accompanied by an increased tone of the sympathetic nervous system (arterial hypertension, coronary heart disease, vegetative vascular dystonia). This leads to the release of a large amount of adrenaline into the bloodstream, which increases the frequency of the generated impulses. Beta-blockers are able to reduce this effect and normalize the pulse, while exerting a pronounced hypotensive effect.
Class representatives are divided into:
- non-selective beta-blockers: Anaprilin (Propranolol), Sotalol;
- selective beta-blockers: Bisoprolol (Concor), Nebivalol, Metoprolol, Atenolol;
- alpha-beta-blockers: Carvedilol, Labetalol.
Anaprilin
Indications:
- arterial hypertension;
- angina pectoris;
- sinus tachycardia;
- myocardial infarction;
- hypertrophic cardiomyopathy;
- mitral valve prolapse;
- vegetative-vascular dystonia;
- combination therapy for pheochromocytoma;
- essential tremor.
Contraindications:
- cardiogenic shock;
- atrioventricular block II-III degree;
- sinoatrial blockade;
- sick sinus syndrome;
- sinus bradycardia;
- Prinzmetal's angina;
- arterial hypotension;
- acute and chronic heart failure;
- severe bronchial asthma;
- Raynaud's syndrome.
"Metoprolol"
Indications:
- hypertension;
- cardiac ischemia;
- myocardial infarction;
- tachyarrhythmias;
- migraine.
Contraindications the same as for "Anaprilin".
"Carvedilol" more effective in cases where rhythm disturbances are associated with chronic heart failure.
Potassium channel blockers
These medications predominantly block potassium channels, but at the same time have an effect on beta-adrenergic receptors.
They are capable of:
- slow down the conduction of impulses through the myocardium;
- reduce the automatism of the sinus node;
- expand the vessels of the heart and fill them with blood;
- reduce pressure.
The most commonly used remedy for arrhythmias from this group is "Amiodarone" ("Cordaron").
Indications:
- ventricular tachycardia;
- ventricular fibrillation;
- atrial fibrillation and flutter;
- paroxysmal supraventricular tachycardia;
- Wolff-Parkinson-White syndrome;
- nodal tachycardia.
Contraindications:
- bradycardia;
- diseases of the thyroid gland;
- sensitivity to iodine;
- fibrosis of the lungs;
- liver failure;
- pregnancy;
- lactation.
Slow calcium channel blockers
These drugs block the flow of calcium through the slow channels into cardiomyocytes. In practice, they are divided into dihydropyridine derivatives (Nifedipine, Amlodipine) and nonhydropyridine derivatives (Verapamil).
The difference between the groups is that the first is capable of reflexively increasing the heart rate, so it is not used to treat arrhythmias!
"Verapamil"
Indications for use:
- paroxysmal supraventricular tachycardia;
- flutter and atrial fibrillation;
- high blood pressure;
- extrasystole;
- vasospastic angina;
- cardiac ischemia.
Contraindications:
- bradycardia;
- sick sinus syndrome;
- ventricular tachycardia;
- tachycardia with a wide QRS complex;
- cardiogenic shock;
- atrioventricular block II-III degrees;
- Wolff-Parkinson-White syndrome;
- arterial hypotension;
- acute myocardial infarction;
- heart failure;
- sinoatrial blockade;
- liver failure.
Other antiarrhythmics
This includes:
- cardiac glycosides: "Digoxin";
- potassium preparations: Panangin, Asparkam;
- metabolic drugs: "Adenosine", "ATP-long", "Riboxin".
Cardiac glycosides are used in cases where it is necessary to arrest supraventricular tachycardia, restore sinus rhythm during atrial fibrillation. But they are contraindicated in bradycardia, intracardiac blockade and Wolff-Parkinson-White syndrome. In case of an overdose, nausea, vomiting, abdominal pain, headache, epistaxis, visual impairment, insomnia as a result of glycosidic intoxication may appear.
Potassium preparations help to reduce the activity of electrical processes in the myocardium. They are used to treat (albeit to a greater extent for prevention) supraventricular and ventricular rhythm disturbances. Side effects: malignant slowing of heart rate, nausea, vomiting, deterioration of atrioventricular conduction.
How to take medications and control your condition?
Every patient taking pills for arrhythmias should be monitored regularly by a doctor. Timely examination allows you to evaluate the effectiveness of therapy, identify side effects in the early stages and take measures to eliminate them. During the examination, the doctor evaluates the following indicators:
- General condition and complaints of the patient.
- Blood pressure numbers.
- Pulse.
- Heart rate.
- Heart rate by electrocardiogram or Holter monitoring results.
- The state of the cardiovascular system according to ultrasound and echocardiography.
- General blood test, coagulogram, biochemical parameters, lipid profile.
- Electrolytes in the blood.
- Renal and liver function tests.
- Hormones.
Conclusions
The main function of the heart is to maintain the necessary blood circulation. Regardless of the cause, a violation of the heart rhythm leads to a significant disorder of the coronary, cerebral and central hemodynamics. Arrhythmias increase the risk of vascular thrombosis (heart attack or stroke). If pathological changes and alarming signs are detected, the specialist will prescribe antiarrhythmic drugs and give recommendations for further prevention of complications.