As a result of untimely treatment of heart disease or low efficiency of its implementation, the patient is at great risk, because the disease tends to become chronic. This also applies to the lack of activity of the main muscle of the body.
Definition and classification
 Chronic heart failure is a disease that occurs more often in middle-aged people. It is a combination of reasons, as a result of which the body ceases to correctly conduct the blood circulation process, to withstand prolonged loads. In this case, the process of fluid retention is often noted.
Chronic heart failure is a disease that occurs more often in middle-aged people. It is a combination of reasons, as a result of which the body ceases to correctly conduct the blood circulation process, to withstand prolonged loads. In this case, the process of fluid retention is often noted.
In chronic heart failure, the balance of the circulatory system is imbalanced, the throughput function of the heart, associated with pumping blood, decreases. This is due to the loss of elasticity of the muscles of the heart and the vascular system.
The New York Heart Association's classification of chronic heart failure is still in use today. It includes 4 functional classes:
- 1st functional class. Heart disease is diagnosed. Physical activity of a person does not have obvious limitations, and does not provoke overwork, heart palpitations, shortness of breath or angina pectoris.
- 2nd functional class. The progression of the disease leads to the manifestation of the first symptoms. Feels limited in physical activity. Fatigue, heart palpitations and shortness of breath begin to appear with standard exertion.
- 3rd functional class. With the further development of the disease, the symptoms become more pronounced. Fatigue, shortness of breath and palpitations are increasingly troubling to the patient, but still do not manifest themselves at rest.
- 4th functional class. A strong limitation of physical activity is felt. Symptoms are felt at rest and are more pronounced with any activity.
Lethal outcome is diagnosed in one third of patients with heart failure of the 3rd and 4th functional classes. There are practically no deaths among patients with functional classes 1 and 2.
 There are also 4 stages of chronic heart failure:
There are also 4 stages of chronic heart failure:
- Initial stage. Impaired blood circulation is not observed, but when examining echocardiography, a deterioration in the work of the left ventricle of the heart is noticeable.
- Stage 2A. The disease has a pronounced clinical manifestation. Disturbed blood circulation in the small or large circle of blood circulation.
- Stage 2B. It is a severe stage of the disease. The mileage is impaired in both circles of blood circulation. Loss of elasticity of the walls of the heart and vascular system.
- Stage 2. The final stage, in which the disturbances in the work of the heart are strongly expressed against the background of severe wear and tear of the muscle tissue of the heart and loss of vascular elasticity.
According to the stagnation of blood in certain parts of the body, the following are distinguished:
- Right ventricular heart failure. Stagnation of blood in the vessels of the lungs, which corresponds to stagnation in the pulmonary circulation.
- Left ventricular heart failure. Stagnant processes in the vessels of the kidneys, brain and heart, in the systemic circulation.
- Biventricular heart failure. Stagnation of blood in both circles of blood circulation.
According to the phases of heart failure, the disease is divided into:
- Systolic heart failure. The period of contraction of the ventricles of the heart is violated.
- Diastolic heart failure. The period of relaxation of the ventricles of the heart is impaired.
Signs
Since the signs of chronic heart disease are extremely diverse, it is not typical for the patient to take its manifestation seriously, for example, accepting slight fatigue or shortness of breath as a natural reaction to physical exertion, while all the symptoms present can be a manifestation of the 1st functional class. Only with the further development of the disease, the patient begins to feel discomfort and worry about his health. The first symptoms of chronic heart failure when diagnosed are:
- dyspnea;
- fatigue;
- increased heart rate;
- recurrent pain;
- swelling;
- characteristic cough.
Chronic heart failure syndrome occurs after prolonged physical exertion. Sometimes it is felt in a state of complete rest. Sometimes shortness of breath can be a harbinger of an impending heart attack.
Fatigue and increased heart rate are natural, this is facilitated by a decrease in the efficiency of the heart and incorrect work of the vascular system, loss of muscle tone.
The appearance of periodic pain is noted in the chest, left side of the body (neck, temple, arm, leg). Patients feel as if they describe the pain as burning or sharp. Pain often makes it difficult to diagnose the disease.
Edema in chronic heart failure warns of blood stasis. The onset of the symptom is characteristic of the stage with clinical severity. Many patients report the appearance of puffiness in the afternoon, but the symptom disappears after a night's sleep. However, this does not prevent the symptom from recurring the next day.
An early cough is characterized by a characteristic dryness, a sign of a lack of retention of fluids in the body. Only the further development of a chronic ailment leads to phlegm, sometimes a cough can be with blood clots.
Causes of occurrence
The causes of chronic heart failure can arise not only in the case of common factors such as unhealthy diet, obesity and the presence of bad habits. The impetus can be:
- Ischemic heart disease resulting from circulatory disorders.
- The onset of myocardial infarction, in which part of the muscle tissue of the heart loses blood flow and dies.
- Arterial hypertension, which is a constant, sustained increase in blood pressure.
- Cardiomyopathy resulting from dysfunction of the muscles of the heart, arterial hypertension and dysfunction of the heart valves.
- Deterioration of the efficiency of the heart as a result of the use of drugs.
- Thyroid disease.
- Endocrine disease.
- Diabetes, difficulty in delivering sugar to the blood.
- Thyroid disease.
- Lack of vitamins.
- HIV.
Risk factors for developing chronic heart failure include:
- arterial hypertension;
- diabetes;
- obesity of various degrees;
- smoking and drinking alcohol;
- renal failure.
Features of childhood failure
Chronic heart failure in children is diagnosed at any age. The symptoms of such a diagnosis in babies are identical to those in an adult, however, the diagnosis of a disease in a child is more difficult, to the extent that the description of well-being by a small patient is limited, especially with the manifestation of the 1st functional class. Newborns with congenital heart disease are closely monitored by doctors. The main thing for parents is to be as aware as possible of the symptoms and nature of the development of chronic heart failure for the timely treatment of the disease in the early stages. Only effective intervention in the development of pathology at this stage can give 100% result. The severity of symptoms and their presence directly depend on the age of the child and the duration of the disease.
To the symptoms of chronic heart failure in children, you can add:
- temporary loss or deterioration of vision;
- loss of consciousness;
- disruption of the vestibular apparatus;
- pallor of the skin;
- blue lips and limbs;
- sleep disturbance;
- constant regurgitation in newborns.
The first signs and symptoms of chronic heart failure occur as a result of normal or increased physical activity. In children under 6 years of age, prolonged, violent crying may affect the manifestation of symptoms. There may be a feeling of suffocation during sleep, shortness of breath at rest. In the presence of a disease in children, physical development and weight gain are impaired. They are extremely difficult to tolerate physical activity.
The effectiveness of the child's treatment depends solely on how quickly this process was started. The principles of treating newborns are to restrict activity, reduce physical activity. To unload the heart, they resort to reducing the amount of water consumed and using a feeding tube. Sedative medicines are used for especially restless babies. The amount of permissible physical activity is discussed with the doctor.
To prevent the development of the disease in children, doctors have to resort to taking medications to increase the contractile functions of the heart. They are glycosides. In the initial stages of the treatment of chronic heart failure, glycosides are administered intravenously. After the symptoms of the disease have subsided, doctors prescribe the glycoside in tablet form.
An important role is played by reducing the load on the heart due to diuretic drugs that help eliminate blood congestion and relieve edema in chronic heart failure. They also add the intake of beta-blockers.
An important role in the treatment of chronic heart failure is played by the use of ACE inhibitors. They are included to suppress the action of cardiac glycosides and reduce the dose of diuretic drugs used.
Diet contributes to the effective treatment of the child. A proper and balanced diet should be rich in potassium.
Diagnostics
Diagnosis of chronic heart failure implies the use of a complex of methods aimed at the timely detection of symptoms and the immediate start of treatment.
First of all, doctors need to know the duration of the onset of symptoms. Also, the emphasis is on the study of the family tree, to find the possibility of a genetic predisposition to the disease. Important information is the patient's possibility of contact with toxic substances, the use of various drugs, the presence of tumors or HIV infection.
Analysis of urine and blood, as well as biochemical analysis is aimed at clarifying the stage of chronic heart failure, cholesterol levels, identifying the process of damage to internal organs.
When using diagnostic methods using ECG, MRI, echocardiography, phonocardiogram, specialists receive information about the degree of heart performance, the correct functioning of the valves, ventricles, and the deterioration of the vascular system and muscles. When examining the structures and functions of internal organs, such as the kidneys and the thyroid gland, doctors assume that the possibility that the development of chronic heart failure is the result of damage or deterioration of the functioning of internal organs is excluded.
Treatment methods
The treatment of chronic heart failure is to follow a strict diet to reduce symptoms and restore correct heart function. The diet should include limiting salt intake (no more than 3 grams per day), liquids (no more than 1.2 liters per day). The diet should contain foods with a high calorie content, but no fat content. It is recommended to eat easily digestible food, which includes cereals and cereals. Strict weight control is required from the patient, since fluid retention is up to 2 kg. over a period of time from one to three days, it may indicate its accumulation in the body and provoking a deterioration in the patient's well-being.
Depending on the degree of neglect of the disease, doctors individually approach the limitation of the patient's mobility and the use of physical activity. A complete rejection of an active lifestyle is unacceptable, but restrictions are possible. The use of exercise therapy exercises, dynamic loads, such as running, swimming, walking, is very useful.
Medicinal methods of treatment include:
- ACE inhibitors, allowing to reduce the development of chronic heart failure, effectively affecting the performance of the heart, vascular system, blood pressure.
- Angiotensin receptor antagonists, if it is impossible to use ACE inhibitors, due to the manifestation of side effects.
- Beta-blockers that help control blood pressure and heart rate.
- Diuretics - diuretics used to get rid of excess fluid accumulated in the body.
- Cardiac glycosides based on plant components, used in small doses for the detection of atrial fibrillation.
With heart failure, treatment requires the use of additional drugs, depending on the causes of the onset and development of the pathology. They are statins, indirect anticoagulants, nitrates, antiarrhythmics.
In the treatment of chronic heart failure, surgical methods are applicable, such as:
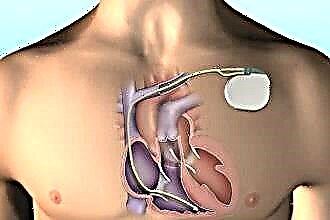
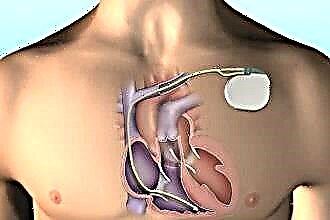
- implantation of a pacemaker;
- coronary artery bypass grafting;
- coronary artery bypass grafting;
- surgical correction of valvular heart disease;
- heart transplant.
One of the most effective surgical methods is resynchronization therapy for heart failure.
What it is? The use of this technique involves the implantation of a pacemaker into the subclavian region of the patient's body and fixation of the implant electrodes on the heart chambers. The implantation process takes up to 2 hours. It is produced using X-ray, for high-precision insertion of the implant into the desired area.
After the implantation, the patient must be in the hospital, under the supervision of the attending physician. Sometimes there is a need for a course of taking medications and in carrying out symptomatic therapy.
Complications
Complications of chronic heart failure can occur both during the natural processes of the development of the disease, and as a result of the low efficiency of the patient's treatment. In the worst case, it can be fatal. Less bad complication options include:
- failure of the heart rhythm;
- degradation of throughput;
- organ enlargement;
- blood clots;
- liver dysfunction.
It is also cardiac cachexia caused by decreased appetite, poor absorption of fats and increased metabolic rate. All of this can lead to weight loss and ulceration of thinned skin.
First aid
The nursing process for chronic failure is the implementation by the nurse of actions aimed at helping patients. This includes providing a favorable environment for the patient to stimulate him in the fight against the disease, informing him in detail about the treatment process and the result, psychological support in difficult times.
These activities include:
- Collection of information. Anamnesis is what can tell the doctor additional information about the patient. First of all, this concerns the diseases he has experienced - they can have a direct impact on the pathology under study. A hereditary predisposition plays a secondary role in this issue.If parents or close relatives have been diagnosed with chronic heart failure, it is highly likely that heredity has become a provoking factor. However, not all doctors think so. Many do not betray her great importance, since they argue that the patient's lifestyle is more important in this matter. If a person works night shifts, drinks alcohol and smokes, then even a good heredity will not save him.
- Compilation of a database of reports in the course of treatment. This is necessary so that the attending physician can trace the dynamics of the development of pathology. The reports show all drugs in exact dosages, injections used in treatment. If the patient's condition deteriorates sharply, then the data in the report will not allow him to re-inject any strong drug, so as not to provoke an overdose.
- Monitoring the patient in a hospital or at home. This applies not only to tracking the dynamics, but also to the patient's well-being. Even subjective feelings and disturbing symptoms matter.
- Patient care planning. It depends on the severity of the condition. In most cases, if the patient remains on outpatient treatment, a nurse comes to him every day and performs the necessary procedures (injections, blood pressure measurements).
- Making a prognosis of the course of the disease;
- Relapse prevention. Prevention of pathology is the task of the patient himself. It depends on how he organizes his day, what he will eat and how to follow the doctor's prescriptions, whether the dangerous symptoms of chronic heart failure will return to him again.
The patient's life expectancy depends on the severity of the disease. Thus, about 75% of patients with functional class 1 survive. This probability is less in patients with the 2nd and 3rd functional classes. The patient's treatment process often ends with a successful recovery or a maximum reduction in destructive processes in the body.