In the context of a constantly deteriorating environmental situation, allergic rhinosinusitis is becoming an increasingly common disease, the age threshold of which is constantly decreasing. If untreated, it leads to the development of chronic diseases and other serious complications.
Reasons for development
 Not always, as the name suggests, it is allergy that triggers inflammation in the sinuses (sinusitis). Quite often the opposite happens - constantly irritated mucous membranes become hypersensitive and give manifestations of allergies at the slightest exposure to previously safe irritants.
Not always, as the name suggests, it is allergy that triggers inflammation in the sinuses (sinusitis). Quite often the opposite happens - constantly irritated mucous membranes become hypersensitive and give manifestations of allergies at the slightest exposure to previously safe irritants.
The development of sinusitis itself can be provoked by:
- congenital or acquired curvature of the nasal septum;
- pathological narrowness of the nasal passages;
- overgrowth of adenoids or polyps;
- any respiratory infections;
- chronic rhinitis of any etiology;
- fungal infections of the mucous membranes;
- bronchial asthma, especially during an exacerbation;
- frequent manifestations of allergic reactions;
- negative impact of external stimuli;
- too dry and hot air in the room;
- sudden or severe weakening of the immune system.
The acute form of the disease is usually provoked by the simultaneous effect of several factors. Then all the symptoms of the disease appear most clearly.
In the absence of treatment, the disease easily turns into a chronic form, and the sensitivity of irritated mucous membranes increases even more, which is the biggest problem for treatment - the range of allergens expands significantly over time.
The main symptoms
Symptoms accompanying allergic rhinosinusitis are typical enough for any respiratory illness:
 profuse watery nasal discharge;
profuse watery nasal discharge;- severe swelling of the nasal mucosa;
- redness and inflammation of the conjunctiva of the eyes;
- red spots and / or skin rashes;
- general weakness, dizziness;
- pain syndrome with a clear localization;
- frequent headaches in the evenings;
- an increase in body temperature up to 38 degrees and above;
- accumulation of mucus on the back of the larynx;
- sore throat, dry, unproductive cough.
Most often, the mucous membranes of the maxillary sinuses and the cells of the ethmoid labyrinth are affected. In this case, the pain is localized on one or both sides of the bridge of the nose and is significantly increased when pressing on the affected area.
If you do not start treatment on time or if pathogens enter the paranasal sinuses, the transparent snot after a while is replaced by thick yellow-green discharge with a characteristic purulent odor.
Diagnosis of the disease
Diagnosing allergic rhinosinusitis can be difficult, and identifying an allergen is even more difficult. This can be done with high accuracy only using modern diagnostic methods. Therefore, after the initial examination, the therapist usually refers the patient for laboratory tests and consultations with other specialists.
The following methods of examination can help to make the final diagnosis and determine the methods of treatment for allergic rhinosinusitis:
- Endoscopy - internal examination of the nasal cavity by introducing a probe into it with a built-in miniature video camera that displays the image on an external monitor. It allows you to assess the condition of the nasal mucous membranes, determine the presence or absence of polyps and other neoplasms, and collect mucus for further research.
- X-ray - a multi-view of the nose allows you to see how far the inflammation has spread and which of the paranasal sinuses are damaged. In some cases, neoplasms become visible in the picture.
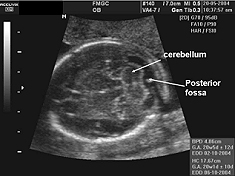
 Ultrasound of the paranasal sinuses is necessary in cases where there is a suspicion that the inflammatory processes in them are provoked by the growth of polyps or cystic formations. It allows you to accurately determine the size and localization of neoplasms and assess the possibility and necessity of their removal.
Ultrasound of the paranasal sinuses is necessary in cases where there is a suspicion that the inflammatory processes in them are provoked by the growth of polyps or cystic formations. It allows you to accurately determine the size and localization of neoplasms and assess the possibility and necessity of their removal.- Computed tomography - is prescribed for complicated allergic rhinosinusitis, when the symptoms are implicit and there is a suspicion that the cause of the pathology is individual anatomical features that are not clearly visible on the X-ray.
- Bacterial sowing of mucus is necessary if there is a suspicion of the infectious nature of the disease and purulent rhinosinusitis. To collect mucus from the frontal sinus, a special probe is used, from the maxillary sinus - an ordinary syringe with a thick needle.
In most cases, one cannot do without consulting an allergist, who also gives a referral for laboratory tests.
They will allow you to determine as accurately as possible which groups of substances cause allergies and the accompanying symptoms. And only after all the results of the examinations have been collected together, the course of treatment is individually selected for each patient.
Drug treatment
There is no general regimen of drug treatment for allergic rhinosinusitis. The drugs are selected strictly individually for each patient. Antihistamines help to quickly remove the manifestations of an allergic reaction, and vasoconstrictor drugs help to reduce abundantly flowing transparent discharge.
Antibiotics are needed only when purulent inflammation of the paranasal sinuses has already developed. Which drug will be the most effective is revealed during bacterial inoculation and depends solely on the nature of the causative agent of the underlying disease.
 Often the difficulty lies in the fact that allergy sufferers have a negative reaction to most antibiotics. Then you have to select drugs by trial and error, checking with caution the patient for the tolerance of each drug. Sometimes an allergic reaction can be significantly reduced or completely suppressed by the simultaneous administration of antihistamines.
Often the difficulty lies in the fact that allergy sufferers have a negative reaction to most antibiotics. Then you have to select drugs by trial and error, checking with caution the patient for the tolerance of each drug. Sometimes an allergic reaction can be significantly reduced or completely suppressed by the simultaneous administration of antihistamines.
In the absence of a strong increase in body temperature, good results are obtained by deep hardware warming of the nasal sinuses. It can be done using ultrasound or infrared radiation. These are different types of influences, each of which has its own indications and contraindications.
- The infrared device creates a powerful directional adjustable beam in the infrared range, which dilates blood vessels, relieves pain and swelling, and facilitates nasal breathing. But this type of treatment is contraindicated in acute inflammatory processes and rosacea - when the blood vessels are greatly dilated or are located very close to the surface of the skin.
- Ultrasound therapy activates the regeneration of damaged mucous membranes due to the impact of high-frequency sound vibrations. It practically does not warm up the skin surface. But with purulent inflammation, this type of exposure is contraindicated. In this case, you must first pump out the accumulated pus from the sinuses and drink a course of antibiotics.
Folk methods
For chronic sinusitis, home treatment with folk remedies is possible, but for an acute form of the disease with an infectious nature, it is not. Therefore, here it is important to start with the correct diagnosis, so as not to waste time on useless procedures and prevent the disease from becoming chronic.
But as auxiliary methods of treatment, folk remedies often give excellent results. Here are some of the most effective ones:
- Decoctions of herbs.Used for rinsing and nasal instillation. The most effective decoctions are chamomile, calendula, St. John's wort, celandine. But here the absence of individual intolerance is important.
 Herbal teas. They should be drunk at least 1 liter a day in a warm form to strengthen the immune system and eliminate toxins as soon as possible. You can brew currant leaves, linden flowers, horsetail, dried raspberries, steam rose petals.
Herbal teas. They should be drunk at least 1 liter a day in a warm form to strengthen the immune system and eliminate toxins as soon as possible. You can brew currant leaves, linden flowers, horsetail, dried raspberries, steam rose petals.- Cyclamen juice. A very effective anti-inflammatory and antibacterial agent. It is enough to instill 3-4 times only 2 drops in each nostril and after a few days there will be significant relief.
- St. John's wort juice. It is not used in its pure form due to its high biological activity - it can cause a burn of the mucous membrane. It is diluted in half with water and dripped 5-6 drops 2-3 times a day.
- Aloe juice. An effective remedy for the healing of affected mucous membranes, quickly relieves inflammation, moisturizes, and has antibacterial properties. Can be used in half with honey for instillation or internal compresses (soak a gauze turunda and add for 10-15 minutes). Not used for purulent inflammation!
It is advisable to treat with folk remedies during pregnancy, or when, for medical reasons, it is not possible to use traditional medicines.
But remember that you still need periodic medical monitoring of how the general condition of the patient changes. And after the completion of the course of treatment, it is advisable to re-take the tests to make sure of complete recovery.
Prevention
Prevention of allergic rhinosinusitis practically does not differ from the prevention of other respiratory diseases, with the only difference that the emphasis is on the state of the air in the room and the absence of external irritants. To do this, it is necessary to regularly inspect the room for the presence of possible allergens, wipe all (including vertical!) Surfaces from dust at least three times a week, and twice a year carry out antifungal treatment of installed air conditioners.
 Additional preventive measures are:
Additional preventive measures are:
- strengthening the body's immune defenses: hardening, vitamin therapy, taking immunomodulators;
- compliance with the optimal temperature regime in residential and work premises;
- regular physical activity, preferably in the fresh air;
- avoiding too sharp changes in temperature and air pressure;
- the use of personal respiratory protection when working in "harmful" industries and in dusty rooms;
- complete natural nutrition, rich in vital vitamins and minerals;
- lack of stress, severe fatigue, optimal sleep and rest.
You also need to see a doctor on time. People often try to treat allergic rhinosinusitis on their own at home first. There is nothing wrong with this, and many folk remedies are quite able to cope with this problem. But if the runny nose does not go away within 7-10 days or the general condition of the patient continues to deteriorate, it is necessary to stop self-medication and go to the doctor for help.

 profuse watery nasal discharge;
profuse watery nasal discharge; Ultrasound of the paranasal sinuses is necessary in cases where there is a suspicion that the inflammatory processes in them are provoked by the growth of polyps or cystic formations. It allows you to accurately determine the size and localization of neoplasms and assess the possibility and necessity of their removal.
Ultrasound of the paranasal sinuses is necessary in cases where there is a suspicion that the inflammatory processes in them are provoked by the growth of polyps or cystic formations. It allows you to accurately determine the size and localization of neoplasms and assess the possibility and necessity of their removal. Herbal teas. They should be drunk at least 1 liter a day in a warm form to strengthen the immune system and eliminate toxins as soon as possible. You can brew currant leaves, linden flowers, horsetail, dried raspberries, steam rose petals.
Herbal teas. They should be drunk at least 1 liter a day in a warm form to strengthen the immune system and eliminate toxins as soon as possible. You can brew currant leaves, linden flowers, horsetail, dried raspberries, steam rose petals.