Causes of pathology
Fibrillation, ventricular flutter occur due to the pathology of the passage of the impulse through the myocardium. These rhythm disturbances are successive stages in the development of one process. In ICD-10 (International Classification of Diseases 10 revision), they are allocated in one heading.
Dysfunction of the cardiac pathways can result from:
- large scar (a consequence of myocardial infarction);
- focal postinfarction cardiosclerosis;
- ischemic heart disease;
- acute myocardial infarction;
- cardiomyopathy with severe cardiomyocyte hypertrophy;
- dilatation (stretching of the walls) of the heart chambers;
- arrhythmogenic cardiomyopathy;
- myocarditis (inflammation of the heart muscle);
- valve defects;
- severe intoxication (including alcoholic vices).
Symptoms and signs of ventricular fibrillation
VF is a life-threatening condition. It develops suddenly, the victim quickly develops a picture of clinical death. However, if he is preceded by ventricular flutter (contraction of muscle fibers with a frequency of more than 200 times per minute), the patient may have time to complain about:
- chest pain;
- a feeling of an accelerated heartbeat (2-3 times per second or more);
- dizziness, loss of orientation in space;
- nausea, which can turn into vomiting;
- increased sweating;
- disturbed rhythm and difficulty breathing;
- general weakness.
These symptoms can last no more than 15-20 seconds. When VF develops, the patient loses the ability to speak coherently. When examining, you need to pay attention to:
- unconsciousness;
- pallor of the skin with acrocyanosis (bluish color of the earlobes, tip of the nose);
- convulsive muscle contractions (occur 35-45 seconds after the onset of an attack, may be accompanied by involuntary urination or defecation);
- a state of clinical death that occurs 2 minutes after the onset of VF, if no help is provided:
- dilation of the pupils (normally they narrow if a person lifts their eyelids in a bright room, but here the opening of the eyes does not cause a physiological reaction);
- it will not be possible to feel the pulse (both on the radial artery (peripheral, passes on the wrist) and on the main artery (large: carotid, femoral);
- breathing stops.
However, to confirm the diagnosis, it is necessary to conduct an instrumental study - electrocardiography.
How does the disease manifest itself on an electrocardiogram?
Ventricular fibrillation on an ECG (electrocardiogram) has several stages of development:
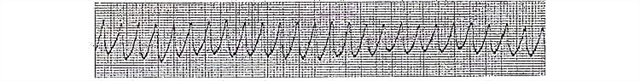
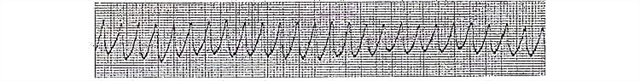
- Flutter of the ventricles. Lasts several seconds, myocardial contractions are still coordinated. On the ECG, it manifests itself in the form of high-amplitude (with a large distance between the upper and lower bending points) rhythmic waves (there can be 250-300 such complexes per minute).
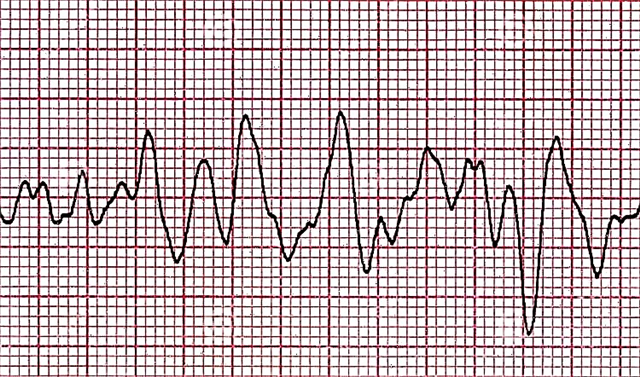
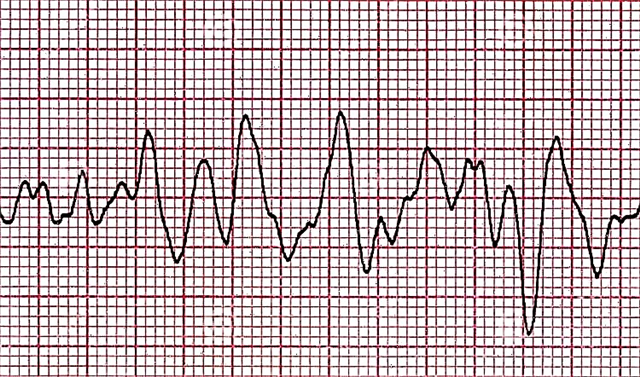
- Convulsive stage. High-amplitude waves remain, but now their frequency is about six hundred per minute. This is a manifestation of a chaotic uncoordinated contraction of individual parts of the myocardium with a duration of 55-65 seconds.
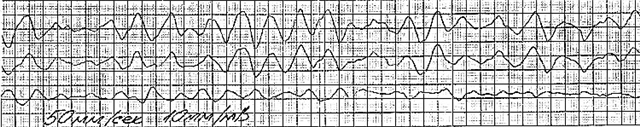
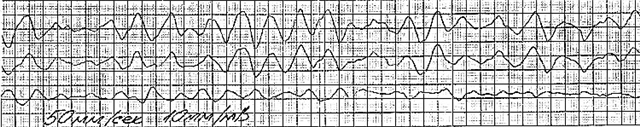
- Flicker of the ventricles. Deterioration of contractile ability leads to an isolated contraction of separate groups of cardiomyocytes. The ECG records small (low-amplitude) waves with a frequency exceeding 100 per minute.
- Atonic stage. The energy reserve of the myocardium is almost completely depleted. There are damped contractions of individual areas of the heart muscle. The waves become even lower and smaller, now their frequency does not exceed 400 per minute.
Photos and examples of films with VF
Let's consider examples of electrocardiographic films and descriptions to them.
- Ventricular flutter

- Stages:
- convulsive;
- atrial fibrillation;
- atonic.

- Convulsive stage
Treatment and care algorithm for VF
Since VF is a condition that poses an immediate threat to the patient's life, there is a documented protocol for action when such a paroxysm occurs. Since the patient is often treated after the transition to a state of clinical death, everything starts with resuscitation.
If a person is found during the convulsive period of VF, then all that is worth doing is to gently keep the head from hitting the underlying surface. Rolled clothing can be used to cushion the effects. It is forbidden to open the victim's mouth, reach the tongue and hold the limbs.
Urgent action
Algorithm of actions in order of priority:
- Check the patient's consciousness: call with a voice, if he does not respond, shake gently by the shoulders (so that the head does not come off the surface on which it lies and does not wiggle along it; the direction of movement is from top to bottom).
- Assess the presence of a pulse. To do this, it is recommended to wrap the fingers of one hand around the central part of the neck (trachea) in the upper half.
- If there is no pulse, call an ambulance (or entrust it to someone).
- Check for breathing. You need to bend your cheek to the victim's mouth and nose, observing the amplitude of the chest movements and at the same time feeling the movement of air with your skin (if any). If necessary, clear the respiratory tract.
- Perform indirect heart massage (in this situation, this is the most important) and artificial respiration.
When the ambulance team arrives, they:
- continue to carry out resuscitation measures;
- connect a cardiac monitor and a defibrillator (in modern models, these two devices are combined);
- after recording an electrocardiogram and confirming the presence of VF, defibrillation is performed (shocks are delivered with increasing intensity every 2 minutes, against the background of chest compressions, until the rhythm is normalized);
In the absence of a defibrillator, it was previously recommended to conduct a precordial blow (with a fist on the lower third of the sternum), but due to injuries and complex execution techniques, it is now not recommended for use.
- if necessary, such medications are administered:
- adrenalin;
- amiodarone;
- lidocaine.
What treatment should a patient with ventricular fibrillation receive?
Emergency ventricular fibrillation should include defibrillation. Depolarization waves roll through the myocardium chaotically, and therefore chest compressions or medications are likely to be ineffective.
When the patient's sinus (normal) rhythm is restored by the efforts of the ambulance team, there is a risk of relapse. To reduce the risk of a second attack, the following drugs are prescribed:
| Group of drugs | Representatives | Purpose of appointment |
|---|---|---|
| Antiarrhythmic | Lidocaine Amiodarone | Prevention of recurrence of ventricular fibrillation immediately after an attack |
| Bisoprolol Nebivolol | Long-term support of an adequate heart rate | |
| Oral anticoagulants | Warfarin Rivaroxaban | Prevention of thrombus formation and embolism (blockage) of blood vessels by them |
| Infusion therapy | Ringer's stereofundin Lactate Trisol Chlosalt Sodium bicarbonate | Restoration of the water-electrolyte balance of the body (it ensures an adequate course of the processes of excitation and contraction in the cells of the heart) |
Are there surgical techniques?
- Implantation of a cardioverter-defibrillator. This device is attached near the left collarbone, and electrodes from it are held to the heart. It monitors the uniformity of the heart rate. When a VF paroxysm occurs, this device delivers a discharge.
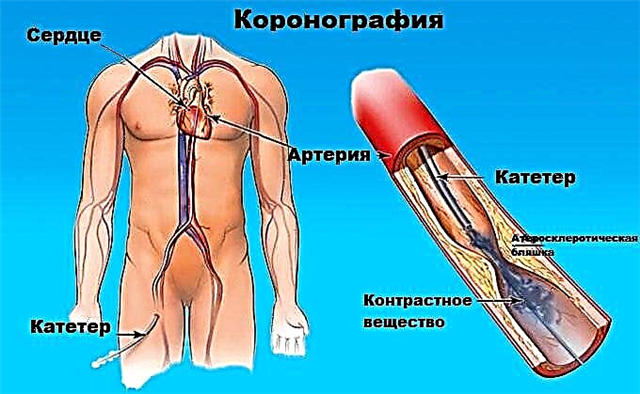
- Coronary angioplasty (stenting of the coronary arteries).If VF has arisen against the background of ischemic heart disease, this surgery will remove the very cause of the paroxysm and prevent relapse.
- Coronary artery bypass grafting (bypass routes to restore blood flow in the pool of one of the coronary arteries). It makes sense if the onset of VF was preceded by an ischemic attack.
How often do you need to come for a checkup with a cardiologist?
Visits to the cardiologist should be carried out:
- As planned, once every 6 months (if the drug treatment for ventricular fibrillation is selected correctly and the heart rate has stabilized).
- Unscheduled. It is necessary to visit a doctor if:
- recurrent arrhythmias;
- presyncopal and syncope states (fainting, dizziness);
- deterioration of health;
- poor tolerance of the prescribed therapy.
How does VF affect life expectancy?
If defibrillation is successful (and it is more effective in large-wave VF), the patient survives and the prognosis for further life is relatively favorable.
During ventricular fibrillation, the myocardium is more susceptible to damage (extensive infarction) due to lack of oxygen (hypoxia). This can lead to an increased risk of sudden death, especially if:
- there is atherosclerotic lesion of the coronary arteries;
- chronic hypodynamia is observed;
- the patient smokes;
- alcoholic beverages are consumed by him often and in large quantities;
- overweight or obese;
- a person suffers from diabetes mellitus;
- arterial hypertension is present, and basic drug therapy is not used.
With properly selected antiarrhythmic therapy, the prognosis for life is favorable.
Conclusions
Irregular contraction of individual muscle bundles in the ventricular myocardium causes their fibrillation. Without immediate cardioversion (restarting the rhythm), sudden cardiac death is very likely.
The clinic is nonspecific: the patient is found unconscious, pale, often with no pulse, breathing and dilated pupils. The criterion for making a diagnosis is a characteristic electrocardiographic picture (waves of different amplitudes).
Specific therapy is a defibrillator discharge. In the future, medical and surgical (if necessary) treatment makes sense.