Description of the syndrome and physiology of its occurrence
In order to understand the essence of the IRR, first I will explain how it arises. The nervous system is divided into somatic and autonomic. The somatic part provides motor responses to external stimuli with the help of the sense organs. For example, when we touch a hot pot, neuromuscular transmission receptors send impulses to pain centers, and we pull our hand back. The vegetative part regulates the activity of internal organs, glands and blood vessels. Thanks to her, our body works like a clock - everything happens involuntarily and on time. Both structural units closely interact with each other and participate in reactions to stimuli at the same time.
Anatomically and functionally, the sympathetic and parasympathetic parts are distinguished in the autonomic nervous system (ANS). The sympathetic part increases our activity, increasing metabolism, as a result of which the excitability of tissues increases. Parasympathetic, on the other hand, helps the body recover by regulating its work during sleep. They function synchronously, but when the "trigger" (most often - stress) is turned on, a dominant is formed - the predominance of one or the other department, which disrupts mental adaptation and emotional balance of a person.

Vegetovascular dystonia is a complex of symptoms arising from dissociation in the work of the autonomic division of the nervous system, manifested by various functional disorders of internal organs and systems.
The syndrome has many synonyms - neurocirculatory dystonia, cardioneurosis, neurasthenia, autonomic neurosis, autonomic dysregulation, dysvegetosis.
Causes
Every day, patients come to see them, in whom I define VSD as the main cause of somatic (physical) disorders. Moreover, in different people, the symptoms can be very different: from movement disorders to a feeling of a lump in the throat. Digging into the causes of the ailments of each individual person, I concluded that there are common factors that provoke vegetative vascular dystonia.
- Family predisposition. If one of the parents has a similar problem, the likelihood of IRR in children increases significantly. The disease often debuts during puberty. Currently, there is no reliable information on the identification of the gene that would be responsible for the presence or absence of the syndrome.
- Diseases of the central or peripheral nervous systems, in which the regulatory centers of the autonomic division are located (increased intracranial pressure due to trauma, tumors, the consequences of a stroke).
- The social environment in which a person is, his relationship with others at home and at work (problems in this sector are often a risk factor).
- Some chronic diseases (endocrine, cardiovascular systems, gastrointestinal tract).
- Change of climatic conditions.
- A history of neuroinfections.
- Features of psychological development.
- Frequent stressful situations, excessive psychological stress.
Symptoms and signs: what the patients come with
The symptoms of VSD are so diverse that the diagnosis can be difficult. It is known that the manifestations of dystonia are "masked" by a large number of diseases. Before visiting me, a neurologist, such a patient has already managed to visit many specialists (cardiologist, gastroenterologist, ophthalmologist). He goes to doctors, takes tests, undergoes examinations, but does not find the source of his ailments. The VSD does not have certain stages, and this delays its diagnosis in some cases.
Depending on the involvement of certain organs or systems, the following types of vegetative vascular dystonia are distinguished:
- Cardiac type characterized by:
- burning, stabbing, pressing pain in the region of the heart (which can be mistakenly perceived as a myocardial infarction), accompanied by shortness of breath, a feeling of lack of air, which do not increase with physical activity, but, on the contrary, become less intense;
- instability of blood pressure, a feeling of fear. In addition to stress, provoking factors can be a change in the weather, the use of alcohol and certain foods. When decoding the ECG, pathological changes are not found.
- Hypotonic type characterized by a decrease in blood pressure (up to 100 mm Hg. Art.), pallor of the skin, sweating, a feeling of lack of air, rapid breathing, nausea, and upset stools.
- Hypertensive type manifested by increased pressure, dizziness, headache, flashing "flies" before the eyes or a feeling of shroud, increased sweating, vomiting, impaired coordination of movements. Doctors are often confused about the symptoms: the clinic imitates a hypertensive crisis, but medications are not needed to stop it - you need to relax, let go of the situation, take a sedative "emergency drug" - and the discomfort will go away. The danger is a prolonged crisis with unrelenting symptoms, in which case I recommend that you immediately seek help from a psychotherapist. And with long-term visual impairment, visit an ophthalmologist to exclude retinal pathology.
- Cerebral type (in some sources - angiocerebral dystonia) occurs when the vascular tone is disturbed, which is manifested by their spasm. Mainly, patients complain of headache, fainting, dizziness, nausea, tinnitus, numbness in the face and limbs. Perhaps the addition of other symptoms - a feeling of chills or fever, shortness of breath, increased heart rate. The most susceptible to this type of dystonia are patients with increased intracranial pressure due to traumatic brain injuries and neoplasms, as well as patients after strokes.
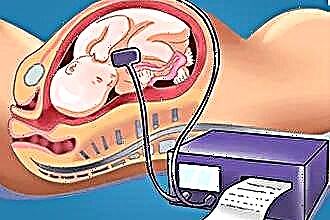
- Wagotonic type characterized by apathy, suspiciousness, loss of memory and attention, pain in the chest and abdomen without clear localization, loss of consciousness, dizziness, cold extremities. Symptoms occur when the vagus nerve (n. Vagus) is activated, which regulates the functioning of organs, glands and blood vessels.
- Mixed type combines the symptomatology of several variants of the VVD and occurs most often.
According to the type of flow, paroxysmal and permanent VSD are distinguished. If the symptoms are observed every day, but their nature does not intensify, we are talking about a permanent course. In my practice, I often come across a paroxysmal form, which is manifested by an abrupt onset, a prolonged peak, a periodic decrease in manifestations, which after a while again intensify. The latter option includes vegetative crises and panic attacks.
Features of manifestations in women
Symptoms and treatment of VSD in adults do not differ much, but the fairer sex is more disposed towards it. In adolescent girls, I observe the appearance of a syndrome due to a mismatch between physical development and the degree of maturity of the nervous system. It is also worth noting that VSD can develop during hormonal changes in the body (pregnancy, postpartum period, menopause). In addition to all of the above, women are more susceptible to emotions, stress and chronic overwork.
The manifestations of VSD in women are mainly:
- heart palpitations, increased blood pressure,
- pressing headache,
- dizziness without impaired coordination of movements,
- increased sweating of the palms and feet,
- feeling of a lump in the throat, lack of air,
- fear, panic,
- lack of appetite,
- muscle pain
- feeling of aching joints,
- the appearance of red spots on the skin of the neck and face,
- increased body temperature,
- general weakness.
If your condition worsens as the weather changes, you are most likely weather-sensitive. Many patients try unsuccessfully to solve this problem by taking a lot of unnecessary drugs. About what this phenomenon is and how to get rid of it, see the video from our expert at the link below.
Case from practice
Approximately 2-3 times a week, I have similar episodes at my appointment, one of which I want to cite as an example.
A 31-year-old woman applied for a consultation. Complains of attacks of a sharply arising feeling of palpitations, shortness of breath, increased blood pressure up to 135/80, periodic tinnitus, dizziness, sleep disturbance, anxiety. She noted a light-headed state twice. The work is associated with constant communication on the phone (operator of the hotline of a government agency), there are frequent conflicts with the management. Attacks are regularly disturbed throughout the year against the background of emotional distress. Comprehensively examined. During the examination, a colleague-therapist recorded an increase in pressure (130/80 mm Hg) and made a preliminary diagnosis of "Hypertension 1 tbsp." According to the data of instrumental examinations - a slight spasm of the vertebral artery on the right, venous outflow is impaired. According to the results of ultrasound of the retroperitoneal organs, pathologies were not revealed. Examined by a gynecologist - pregnancy is excluded.
During a neurological examination: the patient is asthenized, fixed on her own feelings. There is no pathology of the cranial nerves. Reflexes are symmetrical, lively, no pathological. The sensory and motor spheres are not disturbed. In the Romberg position, she is stable, she performs coordination tests well. The limbs are cold to the touch. Excessive sweating.
Diagnosis: "Somatoform autonomic dysfunction, hypertensive type." Taking into account that the symptoms and treatment of vegetative-vascular dystonia in women are necessarily emotionally colored, I recommended: normalizing the daily regimen, regular exercise, daily warm baths with aromatic lavender oils, a course of massage. From medicines prescribed the drug "Afobazol" 1 tablet 2 times a day for a month, followed by a second consultation at the end of the course or in the presence of an exacerbation of the condition.
The patient came to the control after a month and a half. The condition improved markedly, after emotional experiences the signs of VSD ceased to appear.
This example shows well how important it is to find the cause of the discomfort in time and correct it correctly. Symptoms and treatment of vegetative-vascular dystonia in women due to the bright emotional color have their own specifics. Let the young lady relax and rest a little - success will not be long in coming. Men should remember this.
Symptoms of the VSD in men
Men are less likely to complain about vegetative-vascular dystonia. I attribute this to the fact that they are more resistant to stress. However, with overwork, prolonged intellectual overstrain, they also experience autonomic breakdowns. More often, the symptom complex makes its debut in males after 40 years, which is associated with the beginning changes in the hormonal background, alcohol consumption, smoking, spending a lot of time in front of the computer.
Signs of VSD in men are no different from those in women, the severity of manifestations depends only on the degree of lability of the patient's nervous system and his susceptibility to stressful situations. During the neurological examination, I often notice the following symptoms:
- erectile dysfunction,
- visual impairment
- pain in the region of the heart (cardialgia).
How to treat vascular dystonia
VSD may not manifest itself for a long time, but under certain conditions it occurs again, bringing discomfort to my patients. During the appointment, I try to tell you in detail how you can strengthen the vascular response to stress.
Depending on the symptoms of VSD, I recommend:
- physical education at home or sports under the supervision of professional trainers are the most important helpers in the fight against dystonia;
- normalization of sleep and wakefulness (sleep for at least 8 hours);
- adherence to a diet: exclude provocative foods (coffee, alcohol, fried, fatty foods), add vegetables and fruits rich in vitamins and potassium salts to the diet;
- massage courses;
- herbal medicine - aromas of mint, apricot, almond, lavender have soothing properties;
- psychotherapy (the psychosomatic model of dystonia has not been refuted or confirmed);
- Spa treatment.
If the condition does not improve, medication is used. Pharmacies offer a large selection of drugs that patients like to prescribe for themselves, without a doctor's recommendation, which always upsets me. An individually selected drug, taking into account the nature of the dystonia, will certainly give an effect.
What pills do I recommend to my patients to combat VSD:
- Antidepressants are the number 1 drug of choice, they work great for VSD.
- Nootropic drugs - improve energy metabolism in brain cells. Many patients buy drugs, the effectiveness of which has not been proven, for example, "Eltatsin" (we often have disputes with them about the appropriateness of its use in vegetative crises). This bioactive supplement contains amino acids: glycine, glutamic acid and cystine. In some cases, I see it as a preventive measure.
- Anxiolytics, or tranquilizers, have a relaxing effect, relieve feelings of fear, anxiety, anxiety, but have side effects - drowsiness, slow reactions, memory loss, etc. I recommend taking Afobazol to patients with VSD without crises. "Phenozepam" is a stronger drug, so it is preferable to take it under the supervision of your doctor.
- I prescribe angioprotectors to normalize cerebral circulation.
- Antioxidants improve stress resistance. I recommend "Mexidol" if metabolic processes of the brain, blood circulation are disturbed. During my work, patients did not complain of side effects.
As a doctor, I am skeptical about homeopathic medicines - due to the lack of a sufficient number of studies that would show their effectiveness in VSD.
The main thing with VSD is prevention. You can forget about your ailments for a long time and live a fulfilling life. With strict adherence to all recommendations for combating dystonia, it will recede for many months and even years. If you still have questions regarding this syndrome, we recommend that you watch the video below the link. Briefly, accessible and professional about symptoms, diagnosis and treatment from the experts of our portal. Happy viewing!
Doctor's advice: how to live with VSD and what to limit yourself to
- Try to avoid stressful situations.
- If possible, normalize daytime activity and nighttime sleep.
- Exercise at least 2 times a week
- If you feel the approach of an attack, try to relax, if possible, lie down. If the sensation intensifies, consult your doctor, you may need to adjust the treatment or recommendations.
- If the consultation of a psychotherapist or psychiatrist is recommended, do not refuse, visit a doctor, in many cases it is this specialist who will help to deal with your conditions and prescribe effective treatment.
Conclusions
- It should be remembered that the manifestations of vegetative-vascular dystonia are so diverse that they can be mistaken for diseases of organs and systems and undergo treatment for a long time without effect.
- The diagnosis is made on the basis of examination and examination by a doctor.
- Prevention of VSD is effective if carried out regularly.
- Deterioration of the condition is provoked by stressful situations, pregnancy, menopause.
- Treatment should only be carried out under the supervision of a physician.