Etiology
Myocardial dysfunction occurs due to metabolic changes. Metabolism can be influenced by diseases, toxic compounds and external factors. The causes of secondary cardiomyopathy are:
- endocrine diseases;
- infections;
- exogenous intoxication (alcohol);
- accumulation of endogenous toxins (pathology of the kidneys, liver, excess hormones);
- external influence of physical or chemical factors;
- avitaminosis;
- anemia.
Features of certain types of cardiomyopathies
| Type of cardiomyopathy | Provoking factor | Morphological basis | Ways to slow down development |
|---|---|---|---|
| Diabetic | Insulin deficiency and hyperglycemia | Microangiopathy - thickening of the walls of the vessels that feed the myocardium | Control of blood glucose levels, minimization of risk factors (smoking cessation, normalization of body weight, adequate physical activity) |
| Thyrotoxic | Excess thyroid hormones | Inflammation and tissue degeneration | Normalization of thyroid function |
| Climacteric | Estrogen deficiency | Reverse myocardial dystrophy | Regular physical activity, hormone replacement therapy |
| Alcoholic | Ethanol | Damage to cell membranes, fatty infiltration of the myocardium, degeneration of blood vessels and cells of the conducting system | Elimination of alcohol |
Pathogenesis
The general mechanism of the onset of cardiac muscle dysfunction with any nature of the provoking factor is as follows:
- Disruption of the energy supply of cardiomyocytes.
- The work of the regulatory intracellular systems at the highest possible level to ensure the pumping function of the heart.
- Limitation of the reserve capacity of the myocardium. If the use of resources is already turned on at full capacity, then with an increase in the load, there will be no additional return, the reserve has already been exhausted.
- Energy deficiency due to prolonged myocardial hyperfunction.
The heart is adapted to work with the full potential, however, without the possibility of returning to a normal rhythm, the reserves of high-energy compounds ("batteries", energy sources) are depleted.
The decrease in energy production has the following morphological background:
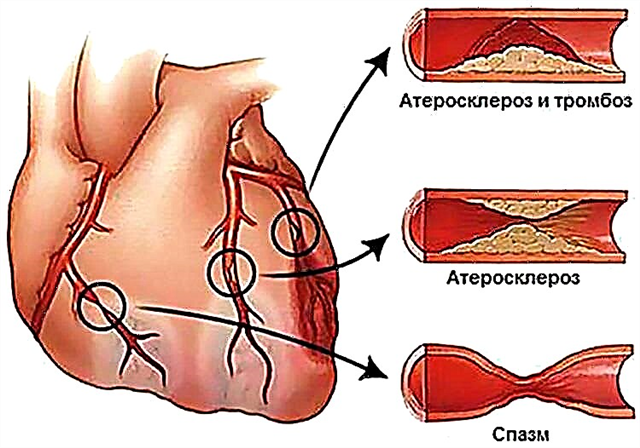
- an increase in the thickness of the capillary wall (it becomes more difficult for oxygen molecules to penetrate into the heart tissue);
- a decrease in the number of vessels per unit volume of the myocardium (leads to a lack of nutrients);
- dysfunction of mitochondria (cell organelles designed to store energy in the form of molecules - macroergs) due to a lack of enzymes, for the synthesis of which oxygen is needed;
- an excess of toxic lipids that destroy the cytoplasmic membranes of cardiomyocytes and trigger apoptosis (self-destruction of cells);
- a shift in pH to the acidic side, which leads to a change in the course of processes that regulate the phases of the cardiac cycle (contraction and relaxation).
Clinic
Clinical symptoms are due to the disease that triggered the onset of secondary cardiomyopathy.
To the symptoms characteristic of the patient's pathology are added:
- pain in the apex of the heart - from top to bottom from the middle of the left clavicle, at the intersection with the fifth intercostal space (in 92% of cases);
- pain in the chest (15%);
- expansion of the boundaries of the heart during percussion examination (the damaged myocardium is stretched);
- muffledness of the first and second tones over all points of auscultation (the heart muscle is softened);
- arrhythmias (violation of intracardiac control over the activity of the conducting system).
Treatment methods and prognosis
When treating, the following points must be taken into account:
- metabolic disorders in cardiomyocytes are reversible only up to a certain point;
- if you do not resume normal metabolism in the myocardium, then heart failure will occur, which is resistant to standard therapy (glycosides).
Thus, the success of treatment depends on whether it will be possible to normalize metabolic processes in the myocardium in time.
Therapy principles:
elimination of the cause (prescription of antibiotics for toxic-infectious processes, replacement or suppressive therapy for endocrine pathology, rejection of alcohol and smoking);
- renewal of adequate energy metabolism:
- extracellular drugs (hormones, blockers and stimulants of the nervous system);
- intracellular drugs (enzymes, cofactors, apoenzymes);
- normalization of the processes of production of high-energy molecules (vitamins of group B, pantothenic and lipoic acids);
- reducing the effect of toxic lipids on cell membranes (antioxidants: tocopherol acetate, nicotinic acid, vitamin C);
- provision of building materials (essential amino acids with anabolic steroids);
- restoration of ionic balance for adequate contractile activity of the heart muscle (potassium and magnesium preparations).
If cardiomyopathic processes are detected at an early stage, the course of treatment lasts 3-4 weeks. If symptoms persist, it is repeated several times a year.
The prognosis is relatively favorable. The ability to work is limited (it is necessary to avoid physical and nervous overload, it is impossible to work with harmful environmental factors). The cause of death in secondary cardiomyopathy can be:
- myocardial infarction;
- violation of the rhythm, up to cardiac arrest;
- pulmonary edema;
- thromboembolic complication.
Conclusions
Secondary cardiomyopathies are often metabolic. Violations of biochemical processes inside the heart muscle occur as a result of intoxication. It can be caused by an excess of hormones, the accumulation of toxic compounds (due to insufficient liver and kidney function), or the action of external agents.
Clinical manifestations are often nonspecific. The absence of cardiovascular disease in the anamnesis is characteristic.
Treatment is aimed at eliminating the cause and restoring the normal course of biochemical processes in cardiomyocytes.