Myocardial infarction is one of the most dangerous diseases of the cardiovascular system, with a mortality rate of up to 35%. I am convinced that statistical indicators can be significantly improved if patients have simple skills in recognizing signs of pathology and providing first aid. Here I want to talk about the leading clinical symptoms of the disease, diagnosis and treatment. This knowledge may one day save lives.
What it is
Let's start with the definition. Myocardial infarction is a necrosis of the heart muscle resulting from an acute violation of the blood supply to the organ. The main factor is the duration of ischemia. If the pain caused by a lack of heart nutrition exceeds 15-20 minutes, then irreversible changes cannot be avoided. In 99.9% of cases, left ventricular infarction develops, since it is he who takes on the entire main load.
By the volume of tissues involved, the following are distinguished:
- large focal or myocardial infarction with a wave of q;
- small focal or myocardial infarction without q wave.
In the presence of a Q wave on an electrocardiogram, the pathology is called Q-myocardial infarction.
Causes
Normally, the heart receives blood through the coronary vessels.
There are a number of factors due to which hemodynamics can be impaired:
- Atherosclerotic lesion of the coronary arteries supplying the heart. In addition to the narrowing of the lumen of the vessels, ulceration of plaques and the imposition of thrombotic masses in these foci are observed, which further aggravate the situation, leading to almost complete occlusion.
- Acute arterial thrombosis. Blood clots most often form in the veins of the lower extremities against the background of prolonged physical inactivity or varicose veins.
- Prolonged spasm of the coronary bed, which occurs against the background of a whole spectrum of pathologies of the central nervous system (craniocerebral trauma, systematic stress, neurosis, etc.)
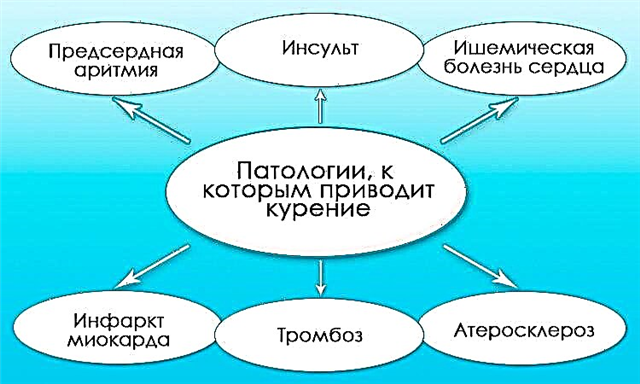
Doctors also identify a number of risk factors that contribute to the development of vascular catastrophe:
- diabetes;
- hypertension or symptomatic arterial hypertension;
- bad habits (smoking, alcohol and drug abuse);
- obesity (body mass index above 30);
- sedentary lifestyle;
- dyslipidemia (increased total cholesterol and LDL cholesterol);
- male gender;
- over 45 years old.
For more information on risk factors and how to deal with them, follow the link.
I'm sure you have at least a few of these criteria. If they are not eliminated in time (most of them can be corrected), then in the future such a formidable complication as myocardial infarction cannot be avoided. Please do not forget that the earlier prophylaxis is started, the lower the risk of developing a serious pathology.
Classification
The principles of the systematics of this disease are many and they differ in different countries. Let us dwell on the main types that are of practical importance.
Depending on the stage of development of necrosis, the following stages are distinguished:
- The most acute - up to 6 hours from the beginning of development. It is during this period that one can try to eliminate the cause of occlusion of the coronary arteries, which will lead to a complete restoration of the vital activity of cardiomyocytes.
- Acute - 6 hours to 2 weeks.
- Subacute - from 14 days to 2 months.
- Scarring period. Lasts up to 5-10 years, in some cases it can be observed for life.
The classification of the disease by stage is based on ECG signs. We will deal with the intricacies of diagnostics later.
Unfortunately, statistics show that the second option occurs only in 20% of cases. With a small lesion, myocardial functions are practically not impaired, and the likelihood of developing fatal complications (aneurysm with cardiac tamponade, acute heart failure) is close to zero. All patients quickly return to their normal life. There were times when they ran away from the department on their own.
Clinical picture
The symptomatology of the disease is extremely diverse.
In the prodromal period (several hours before vascular complications), patients may be bothered by:
- hypertensive crisis;
- an attack of unstable angina pectoris (if there is a history of ischemic heart disease);
- episodes of arrhythmias;
- changes in general condition (agitation, sharp headaches, excessive sweating).
Any changes in the state of the body (especially at the age of 45 and in the presence of serious cardiovascular diseases) should alert. I always recommend that my patients in such situations give up everything, sit down or lie down on the bed, and then measure their blood pressure and pulse. If there are violations, take the appropriate medications recommended in advance by the attending physician, or call an ambulance.
The typical clinical picture is similar in almost all patients.
Pain
The pain syndrome is intense and is always localized behind the sternum. Irradiation may be observed in the left shoulder and forearm, scapula. Less commonly, discomfort in the throat and epigastric region develops.
An important sign is the duration of pain over 15 minutes and the complete or partial absence of the effect of taking "Nitroglycerin". If you experience similar symptoms, call an ambulance immediately. In no case should you take analgesics. They can blur the pain picture and provide an apparent well-being in which necrosis continues to progress asymptomatically.
Dysfunction of the heart
With q-forming myocardial infarction, there may be signs of heart failure from the small (shortness of breath up to 40 respiratory movements per minute, unproductive cough with blood streaks) or large (edema of the legs, pallor of the skin, acrocyanosis, episodes of loss of consciousness) of the circulation.
In the zone of necrosis, there are often zones of impulse conduction, which provide contraction and relaxation of the organ.
ECG for myocardial infarction
In this case, the following are most often observed:
- extrasystole;
- atrial fibrillation;
- AV blockade of any degree;
- heart failure.
Practice shows that with the development of such complications, the probability of a fatal outcome increases several times, since local and general hemodynamics are significantly impaired.
A great danger is posed by atypical forms of myocardial infarction:
- Abdominal - pain in the upper abdomen, nausea, vomiting, bloating. Signs resemble exacerbation of gastritis or pancreatitis.
- Asthmatic. With this option, shortness of breath rapidly increases, resembling the symptoms of bronchial asthma.
- Painless. Patients have only weakness and various manifestations of complications (change in the color of the skin, depression of consciousness). Typical for people with diabetes.
- Cerebral - dizziness, impaired consciousness, delirium, hallucinations.
- Peripheral. With this form, pain in the region of the heart is completely absent, but can be observed in other parts of the body: the left little finger, lower jaw, cervicothoracic spine.
- Edematous... Within a few minutes, swelling of the legs and internal cavities increases with the development of ascites, hepatomegaly.
In the presence of pathologies on the part of the cardiovascular system, any change in the behavior of the body should alert you. Although the frequency of development of such forms is low (over the past year I have met about 20 such patients, which is 1-2% of the total flow of applicants), one cannot ignore them.
Diagnostics
The leading method for recognizing the disease is the ECG, which can be performed after the arrival of an ambulance.
Points of application of electrodes when taking an electrocardiogram
The curve changes differ depending on the stage of myocardial infarction.
Period | Manifestations |
Sharpest | Elevation of the ST segment, the Q wave remains positive. |
Spicy | The appearance of pathological Q, a decrease in the amplitude of the R wave, a slowdown in the rise of the ST segment in comparison with the previous stage. T is either smoothed (located on the isoline) or negative. |
Subacute (time of onset of cicatricial changes) | The Q wave remains, ST comes to a normative position (on the line), T is sharply negative. |
Cicatricial | The presence of Q, the T wave gradually returns to the isoline. |
Expert advice
Now there are many electronic bracelets, which, in addition to showing the time and counting steps, allow you to record an ECG in several leads (as a rule, in two). The points of application of the electrodes are shown in the photo.
If you want to recognize myocardial infarction on your own, then just compare if the line on the electrocardiogram is like a cat's back, where the R wave is the cat's head, the ST segment is the back, and the right side of the T contour is the drooping tail. Take a look at the images. It's pretty simple, isn't it? Q-myocardial infarction will differ only in the presence of a pathological wave.
Identification of the localization of the necrosis focus is of great importance. It is easy to detect by registering the above changes in certain leads:
- side wall - I, aVL, V5, V6;
- partition - V3;
- anterior region - I, V1 and V2;
- lower wall - II, III, avF;
- top - V
Along the way, when studying the electrocardiogram, various rhythm disturbances are determined.
It should be noted that a heart attack without a q wave has some differences. The voltage (distance of raising or lowering) of the ECG elements is much less pronounced, and the main sign of a large-focal lesion (Q) is absent.
Laboratory diagnostics
There are other methods to confirm the diagnosis. These include:
- Complete blood count (there is leukocytosis, increased ESR);
- Troponin test is a marker of striated muscle necrosis. However, it will also be positive if any skeletal muscle is affected.
Both methods can confirm the presence of myocardial infarction only after 6-8 hours and are performed at the inpatient level after hospitalization of the patient.
Instrumental diagnostics
Usually, the matter is not limited to laboratory tests alone. Additional help can be provided by coronography - the injection of a contrast agent into the coronary arteries, which is visualized on an x-ray. The method allows you to assess the localization of the lesion, the degree of occlusion, as well as make a decision on further treatment.
First aid
If you or your loved ones have a similar unpleasant situation, do not panic.
There are a number of things you can do to help alleviate your general condition:
- Call the ambulance team.
- Place the patient on a bed with a raised headboard or place pillows under the back and neck.
- Expose the chest, open the windows. You need as much fresh air as possible.
- Give Nitroglycerin or Nitrospray under the tongue every 5 minutes. It is important to control the pressure before a new dose of nitro drugs. If it is below 100/60 mm. rt. Art. or close to these figures, then the provision of medication should be discontinued. It is also necessary to monitor the heart rate so that it does not exceed 100 beats / min.
- Give Aspirin at a dose of 300 mg.
In no case should you use pain relievers and other medications. They can distort the picture of pain and lead to more serious consequences.
Treatment
If the specialists after examination and ECG diagnosed: "Myocardial infarction", then they urgently hospitalize the patient, providing emergency care in a medical carriage:
- "Acetylsalicylic acid" 0.3 if not previously given;
- "Bisoprolol" 0.0125;
- "Morphine" 1 ml of 1% solution - to relieve pain;
- "Atropine" 0.1% 1 ml - with signs of hypotension and bradycardia;
- "Clopidogrel" 0.3;
- "Heparin" - 70 units for each kilogram of the patient's body weight, but not more than 4,000 units;
- oxygen therapy - for shortness of breath or other signs of respiratory failure.
The patient is delivered to the intensive care unit of the cardiac surgery hospital. If less than 6 hours have passed since the moment of the heart attack, systemic or local thrombolysis is performed. At a later date, coronary artery bypass grafting or wall staging.
Symptomatic therapy is prescribed in the hospital.
Treatment methods:
- Prevention of the development of arrhythmias. Used b-blockers ("Metoprolol", "Atenolol", "Carvedilol"), calcium channel antagonists ("Verapamil", "Amiodarone", "Nifedepine").
- Prevention of thromboembolic complications (Heparin, Ksarelto, Kleksan).
- Pain relief (Fentanyl and Droperidol).
- Prevention of repeated myocardial ischemia ("Nitroglycerin", "Isosorbide dinitrate").
After leaving intensive care (2-3 days), a strict diet is prescribed with a decrease in food volume and its calorie content. Spicy, fried, fatty foods are excluded. Meals should be frequent - up to 6-8 times a day.
Personal experience has shown that patients who did not try to stop anginal pain on their own, but urgently sought medical help, have better chances of a favorable outcome. In 10% of cases, complete recovery of the heart muscle is observed.
Clinical example
There are situations when the clinical picture of myocardial infarction is so poorly expressed that patients do not attach due importance to it and do not seek help from specialists.
Patient D. 59 years old. She came to me for an appointment with complaints of frequent chest pains, the appearance of edema of the legs and an increase in the abdomen in volume, shortness of breath when walking for short distances.
Physical examination revealed an increase in blood pressure (165/105 mm Hg), acrocyanosis, leg edema and ascites. Hearts are heard in the lungs (lower parts), accent II tone over the aorta. The left border of the heart is displaced to the left (2 cm outward from the midclavicular line).
During the examination, the diagnosis was made: “IHD. Stable exertional angina. 3FK. Condition after myocardial infarction. GB 3 tbsp. AG 2 tbsp. P4. H2b. LVD, microalbuminuria ".
The fundamental diagnostic methods were:
- ECG (overload of the right heart, LVH, cicatricial changes after myocardial infarction);
- Echo-KG (hypokinesia of the anterior and lateral walls of the left ventricle, LVD and LVH);
- OAM (microalbuminuria - 0.03 g / l);
- plain radiography of the OGK (congestion in the lungs, increased CTE).
It turns out that the patient in the past (about 4-5 years ago) suffered a myocardial infarction with damage to the anterolateral part of the left ventricle. No therapy was prescribed, the heart areas stopped working adequately, which led to stagnation in the small and large circles of blood circulation due to massive remodeling of the myocardium. Recommended drugs: "Enalapril", "Hydrochlorothiazide", "Nitroglycerin - for pain behind the sternum", "Isosorbide dinitrate", "Mesidol", "Curantil". Such therapy will slow down pathological changes and prolong the patient's life.
Thus, pathology is a serious problem that can take a human life. With myocardial infarction, especially confirmed by an abundance of clinical signs, you should urgently begin providing first aid, having previously called a team of doctors. Only confident actions and complete calmness give hope for success.