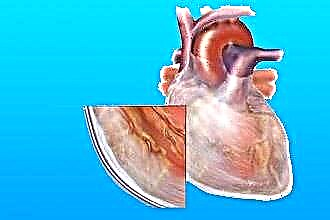
Pericarditis (pericarditis) is an inflammatory process in the serous membrane of the heart. There are 4 types of pericarditis: exudative, adhesive, constrictive and fibrinous (dry). In this article, we will consider the latter in more detail. Fibrinous pericarditis is most common in childhood and adolescence. Its characteristic features are a decrease in the amount of fluid in the pericardium and sweating of fibrin into the cavity of the cardiac sac. Fibrin is deposited on the surface of the pericardium in the form of villi - hence the name “villous heart” in medicine.
The main reasons for the development of pathology
The main etiological factor that leads to the onset of dry pericarditis today is rheumatism caused by bacteria Staphylococcus aureus.
Also, this pathology can occur when:
- infectious diseases;
- transmural myocardial infarction (MI);
- malignant formations;
- actinomycosis;
- tuberculosis;
- autoimmune processes;
- metabolic disorders;
- allergies;
- chest injuries.
Tuberculous lesions arise from translocations of bacteria from necrotic lung tissue or affected lymph nodes into the pericardium.
Fungal etiology of pericardial inflammation is due to the penetration of fungi from the genus Candida into the pericardium. Most often, this type of pericarditis occurs in people with immunodeficiency.
The triggering process for the onset of pericarditis after myocardial infarction is an allergic reaction of the body to the cells of the necrotic myocardium. This is due to the large number of eosinophils in the punctate of the pericardial fluid.
There are 2 variants of postinfarction pericarditis:
- early - appears within a day after myocardial infarction;
- late - Dressler's syndrome - pericarditis is accompanied by pleurisy and peritonitis.
There are times when it is not possible to establish the cause of pericarditis. Then there is cryptogenic dry pericarditis.
Pathogenesis
Dry pericarditis is an acute process that lasts 2-3 weeks on average. After this line, the person either recovers, or the disease is complicated by an increase in the amount of effusion and, as a result, exudative pericarditis develops.
If you look at it, the designation "dry pericarditis" is not entirely correct, since during this disease, plasma sweats into the pericardium. In the next stage, its liquid part is absorbed, and on the surface of the pericardium, the fibrinogen included in its composition is deposited in the form of fibrin. Over time, the thickness of this deposited mass increases, it grows tightly with the layers of the pericardium. When opening, the fibrin strands break, as a result of which the heart has a "villous" appearance, and the pericardial leaves themselves become dull with separate hyperemic areas on them (due to the presence of an inflammatory process).
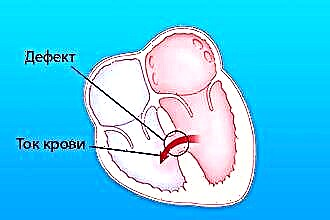
If this type of pericarditis is not treated, or treated incorrectly, pericardial effusion occurs. It is characterized by an increase in the amount of fluid in the pericardium. It accumulates in the lateral cavities of the pericardial bursa and behind it. The heart is pushed forward. Heart failure occurs.
The second variant of complications is also possible - the deposited fibrin leads to scarring, and as a result, the pericardium thickens and its sheets coalesce.
With the right treatment, the fibrinogen masses are completely disorganized by the action of enzymes and are absorbed by the pericardium.
Clinical manifestations
 In the first stage, the disease is difficult to diagnose. Since the symptoms of dry pericarditis include fever, general weakness, increased sweating, decreased appetite and are characteristic of the onset of most diseases.
In the first stage, the disease is difficult to diagnose. Since the symptoms of dry pericarditis include fever, general weakness, increased sweating, decreased appetite and are characteristic of the onset of most diseases.
Pericardial pain is a characteristic sign of pericarditis. It is localized behind the sternum. The strength ranges from mild to similar to angina pectoris. It is manifested by tingling, burning, scratching. The pain becomes stronger in the position on the left side, when inhaling, swallowing, coughing. Weakened by forward bending of the trunk. It can radiate to the left shoulder, scapula, neck, is not stopped by nitrates.
Patients are also worried about paroxysmal coughing, difficulty swallowing. Breathing becomes shallow, accompanied by shortness of breath. In children, hiccups are a common symptom;
A change in the nature of pain is a poor prognostic sign and indicates a transition to the exudative form of the disease. At the same time, the pains resemble angina pectoris, radiating to the back and shoulder blades.
Also, depending on the cause of pericarditis, each patient may have individual symptoms.
Diagnostics
For an accurate diagnosis, the doctor must first take a history and examine the patient.
The characteristic signs of dry pericarditis on examination are a bulging chest wall and smoothed intercostal spaces in children and swollen cervical veins in adults.
Pericardial friction noise is auscultated. It is best heard in the second, third or fourth intercostal space to the left of the sternum along the midclavicular line.
Recall that the main signs necessary for the diagnosis of pericarditis are typical pain syndrome, auscultatory pericardial friction noise and characteristic changes in the electrocardiogram (ECG).
As mentioned above, the cardiogram is one of the mandatory diagnostic measures for the diagnosis of fibrinous pericarditis. When recording an ECG film in such patients, there will be an elevation of the ST segment with its subsequent return to the isoline and the formation of a negative T wave. The same signs are characteristic of myocardial infarction. Distinguishing these two diseases on the EKG allows the absence of a pathological Q wave and the same changes in the three standard leads with pericarditis.
In addition, such patients are prescribed:
- echocardiography - is the most accurate method for diagnosing pericarditis - it allows you to detect the presence of even a very small amount of fluid (from 12 ml) in the pericardium. ECHO-KG also detects changes in heart movements, the presence of adhesions, thickening of the pericardial sheets;
- general and biochemical blood and urine tests;
- immunological tests;
- phonocardiography.
Chest CT or MRI may also be done. These examination methods make it possible to diagnose thickening and the presence of calcification of the pericardium.
Patient treatment and observation
 Fibrinous pericarditis requires complex treatment - etiotropic and symptomatic. It should be carried out in a hospital, since it is necessary to regularly monitor the level of arterial and venous pressure and heart rate. Also, such patients need repeated ECHO-KG for the timely diagnosis of a possible transition of the disease to the exudative form.
Fibrinous pericarditis requires complex treatment - etiotropic and symptomatic. It should be carried out in a hospital, since it is necessary to regularly monitor the level of arterial and venous pressure and heart rate. Also, such patients need repeated ECHO-KG for the timely diagnosis of a possible transition of the disease to the exudative form.
Such patients need diet, vitamins, moderate exercise and immunomodulators to correct the body's immune state.
Drug therapy consists of taking non-steroidal anti-inflammatory drugs (NSAIDs) and glucocortteroids. Can also be assigned:
- narcotic analgesics - in the presence of severe pain syndrome,
- antibiotics - with the bacterial nature of the disease,
- acetylsalicylic acid - if pericarditis was formed against the background of myocardial infarction.
The use of anticoagulants is contraindicated due to possible bleeding in the pericardial cavity.
In most cases, NSAIDs are prescribed.Glucocorticoids are needed in such cases:
- with allergic pericarditis caused by medication;
- with pericarditis of autoimmune genesis.
The GCS dose is selected depending on the cause and complexity of the disease. You should refrain from taking them in case of viral etiology of pericarditis.
For tuberculous pericarditis, GCS is prescribed in combination with anti-tuberculosis drugs. In this case, the patient is led by a phthisiatrician.
If the patient develops heart failure against the background of pericarditis, it is necessary to prescribe treatment with diuretics in combination with a cardiac glycoside.
There are situations when drug therapy is ineffective. Then, to avoid the formation of adhesions between the pericardial sheets, an operation is necessary. The most effective surgical option in this case is pericardiectomy. Its essence lies in opening the chest and draining the pericardium.
Conclusions
In most cases, the outcome of fibrinous pericarditis is favorable. The correct work of the heart is restored in a few weeks. A timely visit to the doctor will help to avoid such negative consequences as the armored heart (so named because of the accumulation of Ca ions in the myocardium, which impede its work) and heart failure (the inability of the heart to perform its main function - supplying blood to organs and tissues of the body).
Since pericarditis is a consequence of other diseases, there is no specific prophylaxis for it. Preventive recommendations are reduced to:
- timely treatment of infectious and chronic diseases;
- avoiding chest trauma;
- strengthening the immune system.
Thus, by controlling the state of your health and referring to a doctor in time, you can maintain your health for many years.