In the general structure of anomalies, congenital heart defects in children rank first (30%) and are one of the main causes of childhood disability. The incidence of pathology in the prenatal period or during childbirth is 1-2 per 100 newborns. Modern diagnostic methods make it possible to establish pathology in the early stages of development and plan the tactics of managing each individual case. The successful application of radical minimally invasive methods of correction makes it possible to eliminate defects in the early stages of a child's growth without irreversible consequences.
Did you know that there are more than 100 types of defects in the structure of the heart and coronary vessels, which are commonly called congenital defects, or CHD? Global statistics claim that the incidence of CHD in children is approximately 8 per thousand. From 0.7 to 1.7% of babies are born with various defects in the structure of this organ. Heart disease in a newborn is a problem that must be addressed. Timely detection and adequate therapy of this anomaly can not only save the child's life, but also give him the opportunity to fully develop.
UPU: an overview
Pediatrics understands congenital defects as violations of the structure of organs or systems that arise in utero. Over a long 40 weeks, the fetus goes through all stages of its development in stages, from a tiny zygote cell to a little man - almost an exact copy of its parents. During pregnancy, all the internal systems of the fetus are gradually formed. Normally, they should develop according to a certain program laid down by nature. And, if everything goes according to plan, at 37-41 weeks the baby is born with fully formed and ready-to-work organs.
It happens that a system debugged by evolution fails. At some point, a breakdown occurs in the usual mechanism, and the organ stops developing according to the plan. It can happen to any internal organ, but we are interested in the heart. It is most vulnerable in the period from the 2nd to the 8th week after conception. At this time, a woman often does not even know about the birth of a new life within her. Any negative influence at this time can be fatal and become a factor that provoked the appearance of CHD.
Why defects appear
We are not reliably aware of the causes of fetal defects. We can only assume the influence of some factors:
- Chromosomal abnormalities are structural or quantitative changes in gene material. Both maternal and paternal cells can be defective. Both a hereditary defect and a mutation that have arisen for the first time are likely. Even if the parents are healthy, for some reason a defect in a single reproductive cell sometimes develops. If this particular cell becomes the basis of the embryo, a violation will occur.
- The influence of external teratogens. Constant contact with toxins is dangerous, especially in the 1st trimester. We often detect CHD of the fetus on ultrasound in women employed in the paint and varnish industry. Taking certain medications in the first trimester (antiepileptic drugs, Ibuprofen, lithium preparations and others) can lead to the same consequences. An excess of vitamin A, ionizing radiation, living in an ecologically unfavorable area are dangerous.
- Intrauterine infections. This is, first of all, rubella - with a primary infection of the body, fetal heart defects, damage to the eyes and the organ of hearing occur. Influenza and cytomegalovirus, any viral infection with fever, are dangerous in the first trimester of pregnancy.
- Maternal factors. The risk of developing CHD in children is higher with a burdened obstetric history. It is always alarming if there were miscarriages before, especially at 13-24 weeks, - a likely consequence of an undiagnosed defect. Alcohol intake by the mother, smoking are fraught with danger for the unborn child. The likelihood of having a baby with CHD is higher in women in labor over 35 years old and with diabetes mellitus.
- Family factors. The use of drugs (cocaine, marijuana) by the baby's father increases the risk of developing CHD.
It is important to know the causes and consequences of heart disease in the newborn and fetus, but it is often impossible to say with certainty which factor was decisive. It is impossible to trace what exactly led to the appearance of the defect. Was the Ibuprofen pill, taken by the mother for a headache, fatal, or was the illness caused by a "caught" virus? We can only assume and try to exclude all negative factors.
The many faces of heart defects: classification and types
The clinical classification of CHD is of interest:
- Cyanotic (accompanied by cyanosis of the skin, mucous membranes). These are Fallot's tetralogy, common arterial trunk, transposition of the great arteries.
- Accompanied by pallor (characterized by vasoconstriction in the skin and mucous membranes). This is the case with patent ductus arteriosus, defects in the septa between the ventricles and atria, and pulmonary valve stenosis.
- Leading to systemic hypoperfusion (weakened blood flow). This is characteristic of aortic defects (stenosis or coarctation).
Another working system involves dividing the CHD according to the characteristics of hemodynamic disorders - blood flow through the vessels. It is important to highlight the following options here:
- associated with fetal communications (features of the fetal blood flow system). The movement of blood in a large circle depends on the patency of a special structure called patent ductus arteriosus, or PDA.
- VSP, not associated with the preservation of fetal structures.
The first case is critical for a newborn. Its circulation depends on how long the foramen ovale and PDA will exist. They have to close during the birth process. Then a full-fledged transition to a new blood circulation regime with two circles is possible. But with this type of CHD, the circulatory system can function only with the preservation of fetal structures - an open oval window or a ductus arteriosus. If they close, a critical situation develops and heart failure occurs.
Symptoms and signs of CHD
Heart disease in newborns can manifest in different ways. The clinical picture depends on the type of defect, the degree of hemodynamic disturbance, the presence of concomitant pathology and other factors. Some congenital heart diseases remain asymptomatic and are not detected during the neonatal period. They are diagnosed later - in infants aged 1-6 months. Less commonly, CHDs are detected after the first year of life.
The leading symptoms of congenital heart disease:
- cyanosis or pallor of the skin and mucous membranes;
- cardiac murmurs;
- signs of heart failure.
During the course of the disease in newborns, two critical periods are distinguished:
- 3-5th day: the oval window closes;
- 3-6 weeks: vascular pulmonary resistance decreases.
During these periods, hemodynamics is impaired, and the child's condition worsens.
In infants and toddlers under 3 years old, the following symptoms may indicate the presence of CHD:
- cyanosis or pallor of the skin;
- fast fatigue when feeding;
- dyspnea;
- lack of weight;
- lag in physical development;
- frequent diseases of the bronchi and lungs.
Some heart defects remain undiagnosed until adolescence. Pathology can be suspected by the following signs:
- lag in physical development (low weight and height);
- fatigue, weakness;
- cardiopalmus;
- swelling of the limbs;
- pallor or cyanosis of the skin;
- excessive sweating;
- cardiovascular syndrome (hoarseness, stridor - wheezing noisy breathing).
If a teenager demonstrates these symptoms, you should consult a doctor: find out the cause of this condition, exclude congenital heart disease.
Clinical case
A baby was admitted for consultation at the age of 3 months. From the anamnesis known: second pregnancy, delivery by caesarean section at a period of 39-40 weeks. Carrying a child proceeded against the background of preeclampsia; in the first trimester, the woman suffered ARVI (she was treated at home on her own).
Congenital heart disease was suspected by a neonatologist in the maternity hospital on the third day after the birth of the baby. The doctor listened to a rough systolic murmur along the left edge of the sternum and referred the child for examination. Echocardiography was performed on the fifth day. Diagnosed with open atrioventricular canal, incomplete form. With this pathology, a defect occurs in the lower part of the interatrial septum, and the bicuspid (mitral) valve also splits.
Supportive therapy was prescribed: cardiac glycosides, diuretics. During treatment, the child's condition remained stable.
A second examination was carried out at the age of 3 months. Based on the results, a decision was made on hospitalization and preparation for surgery. The scope of the surgical intervention is a radical correction of the defect in conditions of artificial circulation. A patch was placed from his own pericardium (the bag surrounding the heart), and the mitral valve was sutured. The postoperative period was uneventful. Upon further observation, the patient's condition remained stable.
Diagnostic scheme
How to examine a child with suspected congenital heart defects? The diagnostic scheme is as follows:
- Physical examination. The general condition is assessed, the pulse and respiratory rate are calculated. The color of the skin and mucous membranes deserves special attention (it is important to identify pallor or cyanosis). Auscultation (listening) of the heart and lungs is performed.
- Instrumental research. If abnormalities are detected during physical examination, an additional examination is indicated. It is necessary to identify a heart defect, establish its type, assess the degree of hemodynamic disturbance.
Auscultation of the heart is a key point in the primary diagnosis of congenital defects. Heart sounds are assessed by a neonatologist at the maternity hospital or by a pediatrician at the reception. It is important to remember that heart murmurs are detected in 60-70% of newborns during the first week of life, but this does not always indicate pathology. Often they are associated with the restructuring of blood circulation and are a variant of the norm.
Murmurs caused by hemodynamic disturbances in CHD are usually detected on the 4-5th day of life or later. Attention deserves noises that persist for more than 3 days, as well as combined with signs of heart failure:
- shortness of breath;
- rapid heartbeat and breathing;
- swelling of the limbs;
- enlargement of the liver;
- increased sweating;
- decreased urine output;
- weak breastfeeding (in newborns and children under one year old).
The absence of a murmur in the heart does not exclude a defect in its development. If there are other symptoms of pathology, it is imperative to examine the patient.
When pathological noises or other signs of CHD are detected, the child is monitored by a cardiologist and the examination continues:
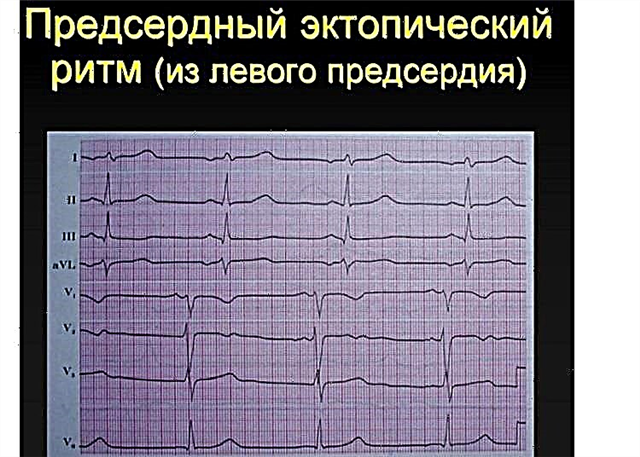
- Electrocardiography (ECG) - an assessment of the main indicators of the heart.
- EchoCG is an ultrasound examination of the heart. On the screen, the doctor sees a two- or three-dimensional image, can identify defects in the development of the heart, assess the blood flow.
- Pulse oximetry - allows you to assess the degree of blood oxygen saturation and identify hypoxia (oxygen deficiency).
- Chest X-ray. It is performed to assess the size of the heart. Helps to identify some defects. The condition of the pulmonary pattern is also assessed. Its changes indicate a violation of blood flow in the small (pulmonary) circulation and help in the diagnosis of many CHD.
- CT scan. Allows you to get a detailed image of the chambers of the heart and nearby vessels. MRI is considered as an alternative.
- Cardiac catheterization. It is carried out only after a complete echographic examination, it gives more detailed information about the work of the organ.

Neonatal screening
According to the protocol, all newborns are advised to carry out pulse oximetry directly in the maternity hospital (or in the neonatal pathology department, if the baby was hospitalized there). The test is performed in the first 24 to 48 hours of life. It allows you to identify undiagnosed intrauterine malformations, including critical ones (CHD, threatening the life of the child). It is allowed to conduct a test on the first day after birth if the baby's condition worsens.
Pulse oximetry is performed by a neonatal nurse. The oxygen saturation (SaO2) is assessed on the right arm and leg. The test results are assessed by a doctor:
- Negative test - SaO2 more than 95% on both limbs; the difference between the indicators on the arm and leg is no more than 3%. This is a good result, it says that the blood flow is not disturbed.
- Positive test - SaO2 less than 95% in one limb and 90-95% in the other, or less than 90% in the arm and leg; the difference is more than 3%. This is an unfavorable result - consultation with a cardiologist and additional examination are required.
EchoCG is considered the gold standard for CHD diagnostics. The full scope of the examination is determined by the attending physician, taking into account the specific clinical situation.
Methods for the treatment of defects
The principle of treatment is determined individually. We take into account the existing protocols, recommendations and determine the tactics of patient management, taking into account the type of defect, the state of blood flow, and other parameters.
Are they taking medications
You cannot get rid of the anatomical defect with pills or injections. We prescribe medications for the child only at the stage of preparation for the operation. Drugs from various groups are used:
- glycosidic cardiac agents;
- ACE inhibitors;
- calcium channel blockers;
- aldosterone receptor antagonists;
- vasodilators;
- diuretics.
The goals of such treatment are to compensate for the resulting heart failure and alleviate the patient's condition. In some cases, drug therapy continues after the operation (especially if the intervention was not radical).
In addition to the main therapy, vitamins are prescribed. Remediation of foci of chronic infection is shown for the prevention of bacterial complications. In case of circulatory failure, oxygen therapy is performed - saturation of the blood with oxygen.
Surgery and indications for it
The operation is required if there is:
- critical congenital heart disease in a newborn;
- signs of acute, congestive cardiac insufficiency;
- severe pulmonary hypertension (increased pressure in the vessels of the lungs);
- a significant decrease in tissue oxygen saturation;
- disruption of the heart valves;
- severe delay in physical development;
- disruption of the work of other organs against the background of heart disease.
Surgical options:
- Radical surgery - complete anatomical correction of the defect, elimination of developmental anomalies.
- Correction of hemodynamics - division of blood flow into venous and arterial. It is carried out if the integrity of the heart cannot be completely restored and the defect cannot be eliminated.
- Palliative surgery is a surgical procedure that does not correct the defect. The purpose of such treatment is to temporarily improve blood flow and avoid the development of complications. Often it becomes a preparatory stage for further radical or hemodynamic surgery.
The table below lists the volumes and terms for the surgical treatment of the most common defects.
UPU | Volume | Terms of operation |
Septal defect between the ventricles | Plastic surgery with a xenopericardium patch, transcatheter occluder closure (steel thread patch) | 1 month with rapid hemodynamic disturbance; 4-6 months with moderate blood flow disturbance; Up to 2 years with compensated CHD |
Atrial septal defect | Radical surgery: repair of a defect with a patch | 2 to 5 years old |
Failure to close the ductus arteriosus | Clipping, ligation of the vessel | 1-5 years |
TMA (mutual displacement of the aorta and pulmonary trunk) | In newborns, the interatrial communication is pre-expanded. Hemodynamic surgery is performed from 3 to 6 months | 1st month, second trimester of 1st year. |
Atrioventricular communication | Radical: atrial septal and leaflet repair | Full form from 3 to 6 months; incomplete form from 1 to 2 years |
Surgical treatment is performed in two ways:
- Closed operation. Possible endovascular intervention, when all manipulations are carried out without incisions, through the vessels. Anesthesia is not required, local anesthesia is sufficient. Closed operations also include operations in which the chest is opened without access to the heart chambers.
- Open surgery. It takes place in conditions of artificial circulation. During the operation, the chambers of the heart are opened. This is how all complex reconstructive interventions are performed.
Consequences: what will happen if not treated?
Congenital heart defect is not a situation that can be left to chance. Without treatment, CHD leads to the development of complications:
- heart failure - a condition in which an organ is unable to do its job;
- violation of the rhythm;
- infective endocarditis - a bacterial lesion of the heart valves;
- bronchopulmonary diseases (bronchitis, pneumonia).
All these conditions significantly disrupt the normal course of life, impede full development and can cause disability.
Prophylaxis
Can the disease be prevented? We do not know for sure why heart malformations occur, and we cannot fully influence this process. But it is in our power to identify pathology at the stage of intrauterine development, to determine the possible risks and prepare for the birth of a child with a defect. If the defect is incompatible with life, termination of pregnancy up to 22 weeks is indicated.
How to give birth to healthy children? Expert advice
Primary prevention is the elimination of all factors that can lead to the birth of a child with a heart defect. For this it is recommended:
- Get the mother-to-be vaccinated against rubella before conception. It has been proven that this disease leads to the appearance of severe CHD in the fetus. You can plan a pregnancy 3 months after vaccination.
- Raise immunity. In the first trimester, the susceptibility to infections increases. It is necessary to take care of the strengthening of the immune system in a timely manner. It is important to monitor your diet, take vitamins in winter and spring.
- Be careful. Avoid self-medication and seek medical attention. Many drugs are prohibited for expectant mothers: they can cause fetal abnormalities.
- To refuse from bad habits. When planning a pregnancy, you should not smoke and abuse alcohol.
- Get treatment. Diabetes mellitus and obesity in a woman increase the risk of developing heart defects in the fetus. You need to lose weight and learn to control blood sugar before conceiving a child.
Secondary prophylaxis is carried out during pregnancy. It is no longer possible to prevent the appearance of congenital heart disease, but they can be detected in the first half of gestation - up to 20-22 weeks. To do this, a woman should regularly undergo prenatal ultrasound screenings at a given time:
- 12-14 weeks;
- 18-21 weeks.
Ultrasound is performed for all patients without exception, but there is a special risk group - those who are more likely to have a child with CHD. These are women who have had a viral infection in the first trimester, are diabetic and obese, who take illicit drugs in the early stages, and are over 35 years old. They definitely should not give up ultrasound - a quick and safe way to diagnose heart defects in utero.
It is important to remember that fetal CHD is often combined with chromosomal abnormalities, therefore, genetic consultation and karyotyping are required.
After detection on ultrasound, he clarifies the diagnosis of FECG. Fetal echocardiography is considered a completely safe method and is performed at any stage of pregnancy.