A phone call made me touch on today's topic. The mother of my 12-year-old patient was extremely excited. Electrocardiography revealed severe sinus arrhythmia in the child. The boy has never been ill for a long time, he plays football. The ECG was carried out as planned on the eve of the next sporting events. And suddenly - such a "terrible" diagnosis. I tried as best I could to convince the interlocutor that her son does not need urgent resuscitation or immediate prescription of medications, and an additional examination must be completed as soon as possible. She asked not to postpone the visit to the reception.
What it is
Let's try to understand what is sinus arrhythmia in a child, why it occurs, how to recognize it, how and when to treat it. Doctors refer to this type of change in heart rate as nomotopic disorders of automatism. The sinoatrial node in this pathology, as in the norm, remains the primary pacemaker, but the formation of the impulse in it is changed.
In the medical literature, the term "sinus arrhythmia" (SA) is sometimes considered synonymous with respiratory arrhythmia, when the heart rate increases during inspiration and decreases during expiration.
Clinical and electrographic classification, proposed by M.S. Kushakovsky and N.B. Zhuravleva in 1981, distinguishes the following violations of the automatism of the sinus node:
- tachycardia - increased frequency of contractions;
- bradycardia - the heart, on the contrary, works slower than normal;
- arrhythmia - an irregular, irregular rhythm;
- rigid sinus rhythm - the number of beats is the same, regardless of physical activity and emotional stress, time of day, state of sleep or wakefulness;
- sinus node failure;
- weakness of the sinus node.

On the electrocardiogram, each complex begins with a P wave, corresponding to one heartbeat. Sinus arrhythmia on the ECG film is reflected by different distances between these teeth. That is, the duration of the intervals from one blow to the next in time is not the same. In this case, the total number of heart contractions in one minute can be equal to the age norm, in contrast to tachycardia and bradycardia.
Age values of heart rate
A baby's heart works harder than an adult's. To clarify the diagnosis of arrhythmia, it is important for a pediatrician to know the rate of heart rate in children.
Domestic and foreign scientists in clinical studies have proven that age-sex values of the number of heartbeats are universal. That is, the heart rate is not affected by:
- race;
- nationality;
- with proportional development of the child - height and weight;
- Country of Residence.
The Center for Syncope and Cardiac Arrhythmias in Children and Adolescents of the Federal Medico-Biological Agency of Russia, based on an expert assessment, has developed indicators that it recommends to pediatricians.
The number of heartbeats in one minute.
Age baby | Newborn | 1 - 2 years | 5 - 7 years old | 12 - 15 years old | 16 - 18 years old | Adults |
Severe tachycardia | more than 160 | more than 175 | more than 130 | more than 110 | more than 110 | more than 110 |
Moderate tachycardia | 141 — 159 | 141 — 174 | 106 — 129 | 91 — 109 | 81 — 109 | 81 — 109 |
Normal indicators | 120 -140 | 110-140 | 80 — 105 | 70 — 90 | 65 — 80 | 60 — 80 |
Moderate bradycardia | 111 -119 | 86 — 139 | 71 — 79 | 51 — 69 | 51 — 69 | 46 — 59 |
Severe bradycardia | less than 110 | less than 85 | less than 70 | less than 50 | less than 50 | less than 45 |
With physical exertion or excitement, the pulse accelerates, and at the time of sleep, it becomes less frequent. Up to eight years of age in boys and girls, the heart beats at the same rate. As they grow older, the main "pump" of the body in the beautiful half of humanity begins to work somewhat faster - by about 5 beats per minute.
Mechanism and causes of SA
Correct heart function depends on the tone of the vagus nerve (vagus). There are two of them in our body. They extend from the brain towards the abdomen, supplying the head, neck, chest, and abdomen. The vagus contains vegetative (regulating the work of internal organs) fibers - both sympathetic and parasympathetic. The sympathetic component stimulates the metabolism, enhances the activity of the heart, the parasympathetic component - reduces the strength and frequency of its beats.
Pathogenesis
Due to the high activity of the autonomic nervous system on inspiration, the atria overflow with blood, the so-called Bainbridge reflex occurs. It consists in an increase in heart rate in response to an increase in central venous pressure (the sympathetic part of the nervous system is activated).
On exhalation, the tone of the vagus nerves increases, which leads to a decrease in the number of heart beats (the parasympathetic fibers of the vagus are turned on). Some authors explain the development of sinus arrhythmia by a compensatory mechanism for improving gas exchange, which reduces the load on the myocardium.
Etiology
Sinus arrhythmia occurs in healthy people and is considered a normal variant if not accompanied by clinical manifestations. The child can be observed after overeating, during sleep; as a result of physical stress - in athletes after training.
Pathological causes:
- Cardiac - a violation of trophism and inflammation affecting the pacemaker (myocardial dystrophy, congenital heart anomalies, myocarditis of various etiologies, circulatory failure).
- Extracardiac - bronchopulmonary and endocrine pathologies, negative effects of certain drugs, micronutrient deficiencies.
- Combined - if cardiac causes are combined with other factors.
I propose to discuss the causes of arrhythmias in adolescents. Metamorphoses of the body during puberty are figuratively called "hormonal explosion" by children's endocrinologists, and psychologists and neurologists who work with teenagers note the lability of their nervous system.
In this age period, arrhythmia is found most often:
- it is in adolescents that autonomic dysfunctions are usually diagnosed, accompanied by a violation of the interaction of the sympathetic and parasympathetic nervous systems;
- we must not forget about coronary artery disease, which, unfortunately, has become "younger" over the past decades;
- wanting to look older, a teenager easily succumbs to the influence of peers, can secretly try alcoholic drinks or drugs, pick up a cigarette;
- young people tend to neglect sleep and rest, sit for long hours at the computer.
Even if your child has no complaints, try to find time for a confidential conversation about adherence to a healthy lifestyle. No matter how surprising it sounds, but taking care of your body is laid in us precisely in childhood, "inherited" from our parents.
How to recognize sinus arrhythmia in a child
You and your child may not be aware of the existence of a heart rhythm disorder. Sinus arrhythmia is often discovered by accident, as happened with my patient.
According to the classification of O.A. Kozyrev and R.S. Bogacheva in 1998, according to the clinical course, cardiac arrhythmias are divided into:
- insignificant;
- significant.
The first "do not bother" the patient. The general condition does not suffer, complaints and clinical symptoms are not observed. The second - significantly complicate life, have an unfavorable prognostic value. This group of arrhythmias requires careful examination and timely treatment.
Complaints and symptoms, or when it is time to see a doctor
The child may complain of a feeling of "interruptions" in the area of the heart, unexplained weakness, dizziness.It is important to understand that preschoolers will not always describe their condition. If you suddenly notice that the baby, who usually runs, sits down to rest, or is experiencing unreasonable fatigue, immediately show him to the pediatrician. This will help you not to waste time with any illness.
The doctor will suspect sinus arrhythmia on auscultation if he hears different lengths of pauses between heart sounds. The pulse will correspond to age, but it will be characterized by inconsistency: within one minute, too fast repetition of beats will be replaced by a slow pace.
ECG signs
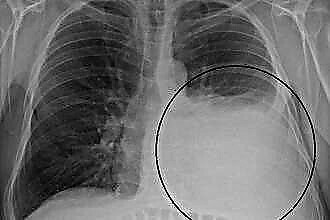
The main diagnostic method for rhythm disturbances is electrocardiography. ECG allows you to clarify the type of change in automatism, conductivity, to identify non-physiological foci of excitation.
Sinus arrhythmia is characterized by:
- constancy of the P wave;
- a gradual increase in the distance between adjacent P or T, and then - the same step-by-step decrease;
- the stability of the PQ interval;
- normal EGC curve when asked to hold the patient's breath.
With Holter monitoring, pronounced sinus arrhythmia in a child will be observed during sleep and physical activity. It is during these conditions that the activity of the vagus increases.
How the doctor and parents should act
Often, parents came to me with complaints that the pediatrician questioned them for a very long time, prescribed numerous examinations, and then said that sinus arrhythmia in a baby or adolescent did not need to be treated. How so? After all, the child has a sick heart. I absolutely agree on this issue with the attending physician.
Survey plan
Sinus arrhythmia does not require special therapy. In some cases, we focus on eliminating its cause - treating the underlying disease. But this pathology sometimes "masks" other disorders. It is important not to miss them.
The examination plan for a child with sinus arrhythmia includes:
- Careful collection by the doctor of anamnesis of life and illness. Do not be surprised if some of the questions asked by the specialist seem strange to you. It is necessary to clarify the genetic predisposition, risk factors, the presence of concomitant pathological processes.
- Electrocardiographic examination. It is important to carry out it at least three times - when the patient is lying down, standing, and then after physical exertion.
- Stress tests. These include bicycle ergometry and treadmills. Thanks to them, it is possible to determine how the work of the heart changes during physical activity, as well as to reveal hidden rhythm disturbances.
- Medicinal electrocardiographic tests. The action of some drugs (in pediatric practice, usually atropine or a combination of potassium chloride and obzidan is used), causes a decrease in the number of heart contractions, which confirms autonomic dysfunction.
- Holter monitoring. Your son or daughter lives at least a day with a portable ECG recorder. The survey will determine the circadian index - the ratio of the average number of heart beats during the day to a similar night indicator. From the age of two, 1.24 - 1.45 are considered normal values. If the index is less than 1.2, this indicates a decrease in vagosympathetic regulation, and with an increase of more than 1.5, an increase in the tone of the vagus nerve. This coefficient is important for the differential diagnosis of sinus arrhythmia.
- Electroencephalography allows you to link the change in the number of heart beats with the bioelectric activity of the brain.
- Echocardiographic examination diagnoses the structural causes of sinus arrhythmias.

Perhaps the doctor will refer the patient to a biochemical blood test, echocardiography, X-ray of the cervical spine, rheoencephalography.
Sometimes viruses are a provoking factor in the development of sinus arrhythmia. Scientists have proven that herpes activates myocardial degeneration. Testing for the herpes virus may be required. Our main task is to clarify the cause of sinus arrhythmia and exclude other changes in heart rhythm.
How to treat
It turned out that the child, whose mother called me, had recently had bronchitis, after a sports training he had a hearty lunch and went to the medical center for examination. Functional tests and Holter monitoring of other cardiac arrhythmias, except for sinus arrhythmia, were not detected in the boy. At the family council, it was decided not to stop training in the football section. As for me, as a pediatrician, I was given a promise to appear in six months for a follow-up examination.
Sinus arrhythmia in pediatric practice usually does not require the appointment of special medications. Try for your child:
- organize an adequate stay in the fresh air;
- exclude a hearty dinner before bedtime;
- provide a comfortable family environment;
- restrict TV viewing and work at the computer;
- stimulate the fight against hypodynamia;
- immunize according to the vaccination schedule;
- teach how to deal with stressful situations at school and in the yard;
- warn against smoking, drugs, alcohol.
Some mothers and especially grandmothers buy vitamins or dietary supplements "for the heart" in order to strengthen the child's body. I strongly advise against doing this without first consulting a doctor.
The parents of my patients sometimes ask whether it makes sense to use traditional methods of treating arrhythmias, in particular with herbs.
Infusions and decoctions are considered overdose pharmaceutical forms. When brewing tea, it is impossible to accurately measure the dose of the active substance that enters the body. In addition, medicinal plants are often allergens, have contraindications, and have side effects.
You have the right to use herbs, dietary supplements or vitamins to improve the functioning of your child's heart, but is there any confidence that you will not harm the health of the growing body?