Prolonged cough in children in most cases is associated not with catarrhal processes in the respiratory organs, but with post-infectious hypersecretion of mucus. The phlegm produced by the mucous membranes of the ENT organs flows down the back of the pharynx, provoking irritation of the cough receptors.
 If the child is constantly gagging in his throat, it is necessary to seek help from a pediatrician in order to accurately determine the cause of the symptom. It should be understood that a cough is a sign that signals the presence of failures in the work of the respiratory system.
If the child is constantly gagging in his throat, it is necessary to seek help from a pediatrician in order to accurately determine the cause of the symptom. It should be understood that a cough is a sign that signals the presence of failures in the work of the respiratory system.
In about 25% of cases, persistent coughing is due to the development of extrapulmonary diseases. The provocateurs of periodic forced expiration can be cardiovascular pathologies, helminthic invasions, allergic reactions, an abnormal structure of the nasal septum, etc.
What is a cough?
Cough is a forced exhalation that occurs as a result of the contraction of the muscles of the airways. A provocateur of a cough act is irritation of receptors located in the paranasal sinuses, trachea, bronchi, larynx, pleura and pharynx, dust, cold air, etc. The impulses generated by the receptors are transmitted by centripetal nerves to the corresponding part of the medulla oblongata. Constant irritation of the pharyngeal mucosa provokes the occurrence of an involuntary physiological reaction, as a result of which the patient begins to cough.
In fact, a cough is a defense reaction that helps cleanse the airways of pathogens and mucus secreted by the ciliated epithelium. In some cases, coughing is caused by hypersensitivity of cough receptors, which occurs as a result of damage to the mucous membranes of the throat, bronchi, trachea, etc. Destruction of tissues is most often due to the development of pathogenic flora in the respiratory organs.
Sometimes the duration of a post-infectious cough is 4 or even 6 weeks.
Causes
 Why does the child often cough? A lingering cough in children is more associated with the anatomical features of the structure of the nasopharynx. Almost all of the discharge from the nasal cavity flows into the airways along the back of the throat, as a result of which irritation of the cough receptors is observed. In decoding a pathological condition, it is necessary to take into account the age and well-being of the child. In infants, coughing can be associated with banal irritation of the mucous membranes of the throat with dust particles and dehydration of the ciliated epithelium.
Why does the child often cough? A lingering cough in children is more associated with the anatomical features of the structure of the nasopharynx. Almost all of the discharge from the nasal cavity flows into the airways along the back of the throat, as a result of which irritation of the cough receptors is observed. In decoding a pathological condition, it is necessary to take into account the age and well-being of the child. In infants, coughing can be associated with banal irritation of the mucous membranes of the throat with dust particles and dehydration of the ciliated epithelium.
The main provocateurs of cough in children include:
- dry air;
- allergic reactions;
- psychogenic factors;
- foreign objects in the airways;
- hypertrophy of the adenoids;
- gastroesophageal reflux.
Coughing with characteristic bubbling rales in the chest may indicate a violation of the evacuation function of the ciliated epithelium.
Most often, a cough reaction occurs in response to the development of an infection in the respiratory system. Pathogens that penetrate the bronchi, trachea, throat and pleura provoke inflammation and, accordingly, irritation of the mucous membranes. As a result, the ciliated epithelium begins to produce more mucus, which irritates the cough receptors and provokes forced exhalation.
Possible diseases
 Coughing is a consequence of a violation of the secretory function of the epithelium lining the inner surface of the respiratory organs. Constant tickling and rawness in the throat provokes an increase in the sensitivity threshold of the cough receptors.
Coughing is a consequence of a violation of the secretory function of the epithelium lining the inner surface of the respiratory organs. Constant tickling and rawness in the throat provokes an increase in the sensitivity threshold of the cough receptors.
For this reason, young children begin to cough at the slightest irritation of the throat with dust, cold or dry air.
The presence of an unpleasant symptom may indicate the development of infectious pathologies, which include:
- bronchial asthma;
- nasopharyngitis;
- adenoiditis;
- whooping cough;
- cystic fibrosis;
- angina;
- bronchitis;
- pharyngitis;
- tracheitis;
- tuberculosis;
- sinusitis.
The inability of young children to cough up mucus is fraught with collapse of the lung and the development of chronic diseases.
Pathological processes in the tissues stimulate the hypersecretion of mucus, which becomes more viscous over time. An unproductive cough in children leads to the accumulation of phlegm in the tracheobronchial tree, which leads to the development of pneumonia. To determine the cause of the appearance of an unpleasant symptom, it is worth considering the etiology and clinical manifestations of common diseases in children in more detail.
Tracheitis
Tracheitis is an inflammation of the ciliated epithelium in the trachea, which most often occurs against the background of acute rhinitis or pharyngitis. The provocateurs of destructive changes in tissues are pathogenic bacteria (staphylococci, meningococci). The development of pathological flora is facilitated by a decrease in local immunity, which is associated with local hypothermia and irritation of the membranes of the airways with dusty or gassed air.
Morphological changes in the tissues of the ENT organs lead to hyperemia and edema of the epithelium, as a result of which there is a hypersecretion of mucus. A common cause of tracheitis is a lingering runny nose, pulmonary emphysema and inflammation of the paranasal sinuses. Hypertrophic changes in tissues increase the sensitivity of the ciliated epithelium, which stimulates the appearance of a cough. Untimely treatment of the disease in young children leads to the development of bronchiolitis.
The characteristic manifestations of pathology is a non-productive cough, which increases with temperature changes, deep breaths and crying of the child. On coughing, sore chest and throat pains. The gradual accumulation of pathological secretions in the area of the tracheal bifurcation leads to the appearance of a paroxysmal cough, which intensifies at night.

Nasopharyngitis
Nasopharyngitis (epipharyngitis) is an inflammatory process in the mucous membranes of the nasopharynx, accompanied by hyperemia, edema and tissue hypertrophy. The defeat of the upper respiratory tract by bacteria and viruses leads to a violation of the secretory function of the epithelium. The mucus flowing down the throat irritates the cough receptors, which causes the child to constantly cough.
With the development of epipharyngitis, children most often complain of the following symptoms:
- headache;
- sore throat;
- persistent runny nose;
- burning when swallowing;
- Difficulty nasal breathing;
- periodic coughing.
Hyperplasia of the lymphoid follicles leads to swelling of the tonsils, resulting in a feeling of a lump in the throat. On examination of the oropharynx, there is redness and swelling of the mucous membranes, as well as granular pharynx. Subsequent intoxication of the body, provoked by the accumulation of pathogen metabolites in the tissues, leads to adynamia, pallor and lethargy of the patient.
Bronchial asthma
 Bronchial asthma is called a sluggish inflammation of the respiratory system, which occurs due to obstruction of the bronchi. The development of pathology is largely due to sensitization of the body and allergic reactions.
Bronchial asthma is called a sluggish inflammation of the respiratory system, which occurs due to obstruction of the bronchi. The development of pathology is largely due to sensitization of the body and allergic reactions.
The characteristic symptoms of bronchial asthma are coughing attacks, shortness of breath, a feeling of congestion and whistling sounds in the chest.
Triggers for spastic cough and exacerbation of the disease are:
- pungent odors;
- animal hair;
- chemical agents;
- sloughing epidermis;
- dust particles.
The high reactivity of the bronchial tree plays a key role in the development of bronchial obstruction.In most cases, sensitization of the body is caused by a disruption in the functioning of the autonomic nervous system, which leads to a decrease in the tone of smooth muscles.
 As a result, there is an increase in the resistance of the airways and, as a result, insufficient ventilation of the lungs.
As a result, there is an increase in the resistance of the airways and, as a result, insufficient ventilation of the lungs.
Focal hypoventilation of the lungs can cause acute asphyxia and death of the patient.
The symptoms of bronchial asthma are similar to those of an allergic reaction. However, it should be borne in mind that not only traditional allergens, but also physical activity can cause coughing in a child. Choking attacks are often preceded by sneezing, hives, and occasional coughing up of small amounts of vitreous mucus.
Cystic fibrosis
Cystic fibrosis is a systemic pathology that develops as a result of mutations in genes responsible for the transport of chlorine ions across cell membranes. Dysfunction of the respiratory system, accompanied by damage to the glandular tissues, signals the development of the disease. Degenerative changes in the lungs lead to the development of chronic bronchitis with bronchiectasis. In children, the disease is often complicated by a bacterial infection, as a result of which mucopurulent exudate begins to accumulate in the bronchi.
Cystic fibrosis is a hereditary disease that is diagnosed in 70% of cases in children during the first 2-3 years of life. The following clinical manifestations signal the development of pathology:
- periodic cough;
- recurrent bronchitis;
- lag in physical development;
- respiratory failure;
- frequent inflammation of the respiratory system;
- chronic sinusitis.
Symptoms can be confused with whooping cough, pulmonary fibrosis, and obstructive bronchitis. Therefore, if characteristic symptoms are found in a child, it is necessary to undergo differential diagnostics by a specialist.
Whooping cough
 Whooping cough is a dangerous bacterial infection that affects the respiratory tract. A characteristic sign of the development of the disease is a spasmodic cough, which can provoke hypoxia and collapse of the lung. Due to the lack of resistance of the body to pathogenic agents, the disease is most often diagnosed in children under the age of 5 years.
Whooping cough is a dangerous bacterial infection that affects the respiratory tract. A characteristic sign of the development of the disease is a spasmodic cough, which can provoke hypoxia and collapse of the lung. Due to the lack of resistance of the body to pathogenic agents, the disease is most often diagnosed in children under the age of 5 years.
Important! A persistent cough can lead to irregular breathing and insufficient blood circulation in the brain.
A highly contagious disease is treated in stationary conditions under the supervision of an infectious disease specialist. To eliminate the pathological flora in the ENT organs, semisynthetic penicillins and macrolides are used. Aerosol therapy and breathing exercises can prevent the appearance of spastic cough.
Adenoiditis
Adenoiditis is called catarrhal or purulent inflammation of the hyperplastic pharyngeal tonsil, which most often occurs against the background of damage to the glands (palatine tonsils). Overgrown adenoids lead to decreased hearing acuity and difficulty in nasal breathing. Hyperplasia of lymphoid tissues most often occurs in children aged 3 to 8 years. The development of pathology is preceded by frequent inflammation of the mucous membranes of the respiratory system, which occurs against the background of influenza, scarlet fever, pharyngitis, etc.
Overlapping the mouth of the Eustachian tube with adenoids is a direct indication for the removal of a hypertrophied tonsil. Adenoiditis is manifested by a dry cough, purulent nasal discharge, severe disturbance of nasal breathing and subfebrile fever. With a timely appeal to the otolaryngologist, the disease can be cured with the help of conservative therapy. Local glucocorticosteroids, as well as anti-inflammatory and anti-edema drugs, can prevent further growth of the pharyngeal tonsil.
Other reasons
 Periodic coughing of a child within a week after the disappearance of the clinical manifestations of ENT disease is considered the norm.
Periodic coughing of a child within a week after the disappearance of the clinical manifestations of ENT disease is considered the norm.
The act of cough occurs due to an increase in the sensitivity of the cough receptors.
After the restoration of the evacuation function of the ciliated epithelium, the unpleasant symptom disappears.
It should be noted that forced expiration can occur due to the development of extrapulmonary diseases. Quite often, coughing is due to the following reasons:
- teething;
- helminthic invasions;
- allergy;
- dysphagia;
- gastrointestinal reflux.
Particular attention should be paid to the psychogenic causes of the cough. A psychogenic cough is the body's response to stress in kindergarten, school, family, etc. A cough with a metallic tinge intensifies when psycho-emotional overstrain occurs. Over time, the consolidation of the cough syndrome is observed, as a result of which the child begins to cough even in the absence of psychogenic stimuli. Such patients require careful examination by a pediatrician to exclude infectious diseases, and in some cases, trial therapy with steroid sprays.
Diagnostics
The choice of methods and drugs for the treatment of cough largely depends on the results of the diagnosis. The appearance of an unpleasant symptom is not always due to respiratory diseases and post-infectious complications.
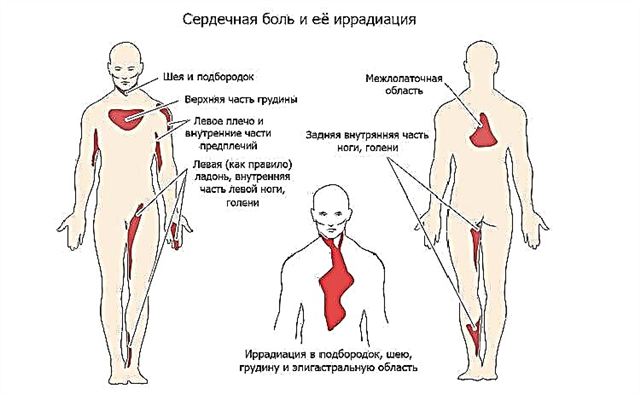
 Periodic coughing can signal the presence of systemic failures, the development of cardiovascular pathologies, helminthiasis, pharyngeal neurosis, etc. To determine the main causes of cough syndrome, a specialist must analyze the following information:
Periodic coughing can signal the presence of systemic failures, the development of cardiovascular pathologies, helminthiasis, pharyngeal neurosis, etc. To determine the main causes of cough syndrome, a specialist must analyze the following information:
- the duration of the cough;
- the amount and properties of mucus separated from the ENT organs;
- the presence of concomitant symptoms;
- the dependence of the cough reaction on the season;
- previous infectious diseases.
Cough syndrome is a complex diagnostic problem, since not only respiratory diseases, but also many extrapulmonary pathologies can provoke the appearance of a cough reaction. To determine the cause of the symptom, a visual examination of the mucous membrane of the oropharynx, X-ray examinations, general and biochemical blood tests allow. A high concentration of immunocompetent cells in the blood most often signals the development of an infectious disease. The bacterial culture from the pharynx allows to determine the nature of the causative agent of the infection.
Treatment principles
What if the child coughs? It should be noted that the act of cough is one of the protective and adaptive reactions, therefore, the main task of drug therapy is not to eliminate, but to alleviate the symptoms of the disease.
Cough suppressants are used only in the absence of mucus discharge during forced expiration. Unproductive coughing fits can lead to nausea, vomiting, or choking.
As part of pharmacotherapy to eliminate cough syndrome, the following types of medicines are used:
- antitussives - reduce the sensitivity of cough receptors or inhibit the activity of cough centers;
- mucolytic - reduce the viscosity of mucus in the bronchi, which facilitates its evacuation;
- expectorants - stimulates the removal of pathological secretions from the respiratory tract;
- muco-regulating - affect the secretory function of the ciliated epithelium, which allows
 regulate the amount of mucus that separates.
regulate the amount of mucus that separates.
Children should not be given antitussives during a productive cough, as this will lead to the accumulation of mucus in the bronchi.
Mucolytic and antitussive agents can only be prescribed by a specialist after the patient has undergone an examination.
It should be noted that even in the absence of phlegm during coughing, antitussives can be used for no more than 3-4 days in a row.
Antitussive drugs
Antitussives are prescribed only when the act of cough is not physiologically justified. In pediatric therapy, to eliminate an unpleasant symptom, mainly non-narcotic drugs of central action are used. They suppress the activity of cough centers, which interferes with the processing of signals from the corresponding receptors.
Effective antitussive drugs include:
- "Sinekod";
- "Panatus";
- Libeksin;
- "Bronchoton";
- "Glycodin".
To speed up the action of drugs, tablets and drops should be given to children before meals.
Drugs that stop a cough reaction are prescribed for whooping cough, pleurisy, flu and other colds. A prolonged unproductive cough leads to overstraining of the pharyngeal muscles, therefore, untimely relief of the symptom can lead to smooth muscle spasm and suffocation.
Mucolytic drugs
Secretolytic (mucolytic) agents affect the gel phase of sputum, which contributes to their liquefaction and evacuation. Drugs in this group stimulate the excretion of mucopurulent secretions that occur during the development of sinusitis, chronic rhinitis, sinusitis, etc. Contrary to popular belief, mucolytics do not lead to an increase in sputum volume, so they can be used to treat preschool children.

To eliminate wet cough in pediatric therapy, the following secretological preparations of reflex action are used:
- "Acetylcysteine";
- Bromhexine;
- "Lazolvan";
- Ambrobene;
- "Fluimucil";
- "Kashnol";
- Bromhexine.
Sputum is a breeding ground for most disease-causing microbes. Cleansing the tracheobronchial tree from pathological secretions inhibits the further development of pathogens, which speeds up the healing process.
General recommendations
Post-infectious cough is caused by hypersensitivity of cough receptors. To eliminate an unpleasant symptom, it is necessary to eliminate the maximum number of provoking factors that irritate the cough receptors. This requires:
- wipe the dust in the room every day;
 provide the child with plenty of drink (warm tea, herbal decoction, fruit drink);
provide the child with plenty of drink (warm tea, herbal decoction, fruit drink);- use humidifiers;
- ventilate the nursery at least twice a day.
During treatment, it is advisable to limit the child's contact with pets, whose fur can provoke irritation of the throat mucosa. In the heating season, before going to bed, you can put a bowl with a decoction of chamomile or sage next to the child's bed. Evaporation of medicinal decoctions will prevent drying out of the mucous membranes and, accordingly, irritation of the cough receptors.

 regulate the amount of mucus that separates.
regulate the amount of mucus that separates. provide the child with plenty of drink (warm tea, herbal decoction, fruit drink);
provide the child with plenty of drink (warm tea, herbal decoction, fruit drink);