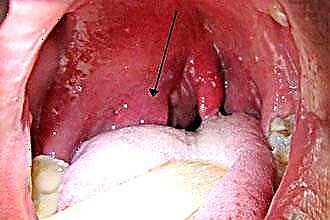
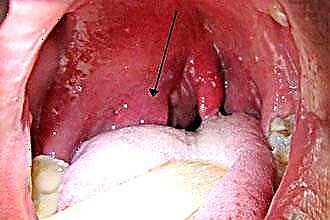
The defeat of the glands and the posterior pharyngeal wall by an inflammatory process with a purulent component, as well as the activation of the fungal flora, leads to the appearance of a white plaque on the mucous membrane. The points on the tonsils represent suppurative follicles that are observed with follicular angina.
 On the tonsils and on the throat, white spots may indicate diphtheria, pharyngomycosis, chronic or acute tonsillitis, as well as specific types of tonsillitis, such as candidiasis.
On the tonsils and on the throat, white spots may indicate diphtheria, pharyngomycosis, chronic or acute tonsillitis, as well as specific types of tonsillitis, such as candidiasis.
Diphtheria
Infection and reproduction of Leffler's rods leads to the development of diphtheria with localization of the pathological focus in the oropharynx, although damage to the nose, eyes and genitals is also possible. Distinguish between a limited form of catarrhal, insular type with the formation of films, and toxic of three degrees of severity.
Symptomatically, the disease manifests itself:
- a rapid rise in temperature to a febrile level;
- malaise;
- drowsiness;
- decreased appetite;
- increased heart rate;
- pain syndrome in the oropharynx.
Hyperthermia is observed for 3 days, during which white dots cover the mucous membrane of the glands. Then white spots appear on the tonsils and pharynx, which indicates the progression of the disease and the spread of the infectious-inflammatory process.
The films become denser, with a pearlescent sheen, are difficult to remove, leaving bleeding wounds. The next day, a speck with a bloom appears at the site of the wound. On the 5th day, the plaque becomes friable and is easily removed from the surface of the mucous membrane.
Closely located lymph nodes increase due to swelling, and also become sensitive to palpation. In the case of the catarrhal form, the intoxication syndrome is not so pronounced, and the sore throat is moderate.
In 4-10% of cases, the limited form becomes widespread, covering the larynx and pharynx. Pharyngoscopy reveals white spots on the back of the throat, as well as white spots on the tonsils, arch, tongue, and palate.
To date, the most common is the toxic form of pathology, in which recorded hectic hyperthermia, heart palpitations, severe intoxication syndrome, decreased blood pressure and cyanosis of the lips.
recorded hectic hyperthermia, heart palpitations, severe intoxication syndrome, decreased blood pressure and cyanosis of the lips.
Intoxication leads to disorders of the nervous system, hallucinations, impaired consciousness and breathing.
Severe edema of the oropharynx and larynx contributes to the growth of shortness of breath, respiratory failure and asphyxia.
With damage to the larynx, croup develops, which has three stages:
- dysphonic, in which there is a rough, "barking" cough, hoarseness, after which aphonia develops;
- stenotic, when there is pallor of the skin, noisy breathing and anxiety;
- asphyxia, characterized by shortness of breath, arrhythmic breathing and respiratory failure.
Among the complications should be highlighted:
- infectious toxic shock;
- nephrosis;
- adrenal insufficiency;
- polyradiculoneuropathy;
- myocarditis.
Diagnostics consists in instrumental and laboratory examination. Bacteriological examination of smears and culture can determine the type of pathogenic microorganisms, as well as their sensitivity to drugs. To assess antibodies, RNGA and PCR are performed. In the process of laryngoscopy, swelling, redness of the mucous membrane, fibrinous plaque in the lumen of the larynx and trachea are visualized.
Angina
The defeat of the lymphoid tissue by the inflammatory process in the oropharynx is often localized in the palatine tonsils. Infection occurs by air and contact. Primary tonsillitis develops as a result of human infection and direct damage to the glands. Secondary, the tonsils are damaged by mononucleosis, diphtheria, scarlet fever, candidiasis and activation of the spirochete.
In 90% of cases, tonsillitis is a consequence of bacterial infection with streptococcal pathogens. Infection with staphylococcus, pneumococcus or Haemophilus influenzae is also possible. The viral origin of tonsillitis is due to the course of parainfluenza, influenza or adenovirus infection.
Predisposing factors include decreased immunity, smoking, dryness, dustiness, hypovitaminosis and general hypothermia. There are several forms of angina (follicular, lacunar, necrotic, ulcerative-film), however, white spots on the tonsils are observed only in the first two forms:
- for follicular sore throat is characterized by moderate intoxication, febrile hyperthermia, pain in the oropharynx, aggravated by swallowing. With pharyngoscopy, there is swelling, hyperemia of the mucous membrane, white dots, which are suppurating follicles. When they are opened, the purulent discharge comes out and covers the tonsils with a yellowish film;
- with follicular - the formation of purulent plugs in the lacunae is observed. With pharyngoscopy, a film is recorded on the tonsils, caused by a purulent plaque. When the process spreads to the pharyngeal wall, a white spot is visualized on the throat wall. Clinically pathology manifests itself
 hectic hyperthermia, severe intoxication syndrome and pain in the oropharynx.
hectic hyperthermia, severe intoxication syndrome and pain in the oropharynx.
From infection to the onset of symptoms, it takes up to 3 days, after which the fever rapidly increases, chills, malaise, photophobia, body aches, drowsiness and regional lymphadenitis (soreness, sensitivity of the lymph nodes) appear. Among the complications, it is worth highlighting:
- otitis;
- paratonsillar abscess;
- peritonsillitis;
- rheumatism (cardiac defects, myocarditis, endocarditis, renal dysfunction, polyarthritis).
For diagnostics, pharyngoscopy is used, in which white dots, loose, infiltrated tonsils, hyperemia of the mucous membrane and an increase in lacunae with purulent contents are revealed. To confirm the diagnosis, a bacteriological examination and culture are prescribed, which make it possible to determine the type of infectious microorganisms, as well as their resistance to antibacterial drugs.
Fungal infection
The activation of opportunistic fungi leads to the development of fungal infections. Reproduction of candida fungi is often diagnosed, but molds are detected in 5% of cases. The appearance of disease-causing properties in fungi is due to:
- a decrease in immune defense as a result of an exacerbation of severe somatic pathology, with cancer, tuberculosis and ARVI;
- long-term use of glucocorticosteroids, antibacterial drugs in large doses, long course;
- radiation and chemotherapy.
Clinically, candidal tonsillitis has no pronounced symptoms. Endoscopic techniques are used in the diagnosis. In the process of pharyngoscopy, white spots in the throat and glands are revealed in the form of plaques. Also, the fungal process can spread to the cheeks and tongue. Plaques are easily removed from the mucosal surface.
To confirm the diagnosis, a mycological study is required, which makes it possible to identify pathogenic pathogens and establish their sensitivity to medications. Therapeutic tactics are aimed at eliminating the provoking factor and prescribing antimycotic drugs (Intraconazole, Fluconazole). Local therapy consists in flushing the lacunae with a nystatin solution.
Local therapy consists in flushing the lacunae with a nystatin solution.
As for candidal pharyngitis, it manifests itself symptomatically:
- discomfort, burning sensation, soreness in the oropharynx;
- dryness, unpleasant odor;
- moderate pain syndrome, which is aggravated by eating food with spices;
- subfebrile hyperthermia (extremely rare).
Recently, fungal infection has been diagnosed quite often among otolaryngological pathology. Given the variety of clinical and morphological properties, there are several forms of pharyngomycosis:
- pseudomembranous, characterized by the appearance of raids of a white-yellow hue;
- erythematous, which is manifested by hyperemic areas with a varnished surface;
- hyperplastic, when white plaques form, the removal of which is difficult;
- erosive-ulcerative, in which ulceration of the pharyngeal mucosa of the superficial type is observed.
With pharyngoscopy, swelling of the mucous membrane, a white spot in the throat and plaque is recorded. The lesions are localized mainly on the tonsils, pharyngeal wall and arches. The deposits are white in color and have a curdled consistency. They are easy to remove, but sometimes they can leave a bleeding surface.
When the candidiasis process spreads to the surrounding tissues, damage to the larynx, esophagus and tongue is noted. Differentiation is carried out with diphtheria. With inadequate treatment, the risk of an abscess in the oropharynx and the development of sepsis increases.
Complicated fungal pharyngitis requires hospitalization. In the treatment, antifungal therapy of systemic action is used. Topically, rinsing, washing the tonsils and pharyngeal wall with antiseptic solutions (Miramistin, Clotrimazole) is prescribed.
The key to success in the treatment of fungal infection is to increase the immune defense and treat concomitant severe pathology.
Prevention of damage to the tonsils and throat consists in maintaining oral hygiene, regular sanitation of chronic infectious foci in the nasal and oropharynx, strengthening immunity, proper nutrition, timely treatment of somatic diseases and quitting smoking. By following the recommendations, you can not only prevent diseases of the ENT organs, but also generally improve your health.

 hectic hyperthermia, severe intoxication syndrome and pain in the oropharynx.
hectic hyperthermia, severe intoxication syndrome and pain in the oropharynx.

